Pediatric Disaster Toolkit
View Adobe Acrobat Version | Download Adobe Acrobat Reader
Hospital Guidelines for Pediatrics in Disasters
2006 1st Edition
Draft for Public Comment
Comment Period May 1, 2006 - June 30, 2006
Created by:
CBPP Pediatric Task Force &
NYC DOHMH Pediatric Disaster Advisory Group
Copyright © 2006
New York City Department of Health and Mental Hygiene
New York City, NY 10013
First Edition
This publication was supported by Grant Number U3RHS05957-01-00 from the Health Resources and Services Administration. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of HRSA.
All inquiries about the “Pediatric Tool Kit: Hospital Guidelines for Pediatrics in Disasters”
may be addressed to:
Bioterrorism Hospital Preparedness Program
c/o NYC Department of Health and Mental Hygiene
125 Worth Street, RM 222, Box 22A
New York, NY 10013
Phone: 212-788-4277
List of Contributors
The following contributors comprised the Centers for Bioterrorism Preparedness Planning (CBPP) Pediatric Task Force.
George L. Foltin, MD
Co-Chair CBPP Pediatric Task Force
Associate Professor of Pediatrics &
Emergency Medicine
Bellevue Hospital Center/
New York University School of Medicine
Bonnie Arquilla, DO
Co-Chair CBPP Pediatric Task Force
Assistant Professor of Emergency Medicine
Director Emergency Preparedness
SUNY Downstate/Kings County Hospital Center
Katherine Uraneck, MD
Project Manager/Editor
Surge Capacity Medical Coordinator
Bioterrorism Hospital Preparedness Program
NYC Department of Health & Mental Hygiene
Silka Aird
Assistant Director of Safety
Bellevue Hospital Center
Mary Caram, LCSW
Associate Director of Social Work
Bellevue Hospital Center
Esther Chackes, DSW
Director of Social Work
& Therapeutic Recreation
Bellevue Hospital Center
Arthur Cooper, MD, MS
Professor of Surgery
Director Trauma & Pediatric Surgical Services
Harlem Hospital Center
George Contreras, MPH, MS, EMT-P
Director of Emergency Management
NYU Medical Center
Christopher Freyberg, MD
Emergency Medicine
VA New York Harbor Hospital System
Robert Hessler, MD
Assistant Director of Emergency Services
Bellevue Hospital Center
Jeffrey Hom, MD
Assistant Director of Emergency Services
Associate Professor of Emergency Medicine
SUNY Downstate Medical Center
Ann Kehoe, MS, RD, CDN
Assistant Director Clinical Nutrition Services
Bellevue Hospital Center
Pamela Kellner, RN, MPH
Infection Control Coordinator
Emergency Readiness & Response Unit
Bureau of Communicable Disease
NYC Department of Health & Mental Hygiene
Stephan A. Kohlhoff, MD
Assistant Professor, Pediatrics
Division of Pediatric Infectious Diseases
SUNY Downstate/Kings County Hospital Center
Jessica Kovac
Administrative Director
Emergency Department
NYU Medical Center
Gloria Mattera
Director of Child Life & Development Services
Bellevue Hospital Center
Kristin Montella
Coordinator
New York Center for Terrorism Preparedness
Bellevue Hospital Center
Evan Nadler, MD
Director of Minimally Invasive Pediatric Surgery
New York University School of Medicine
Nooruddin Tejani, MD
Director Pediatric Emergency Medicine
SUNY Downstate Medical Center
Michael Tunik, MD
Associate Professor
Pediatrics and Emergency Medicine
Director of Research Pediatric Emergency Medicine
Bellevue Hospital Center
Ellen Webb
Coordinator
New York Center for Terrorism Preparedness
Bellevue Hospital Center
Pediatric Disaster Advisory Group Members
Samuel Agyare, MD
Director of Pediatric Emergency Medicine
Woodhull Medical and Mental Health Center
Robert van Amerongen, M.D., FAAP, FACEP
Chief, Pediatric Emergency Service
Department of Emergency Medicine
New York Methodist Hospital
Oxiris Barbot, MD
Assistant Commissioner
Bureau of School Health
NYC Department of Health & Mental Hygiene
Debra Berg, MD
Director Bioterrorism Hospital Preparedness Program
Bureau of Communicable Disease
NYC Department of Health & Mental Hygiene
Nelly Boggio, MD
Director of Pediatrics
Emergency Management
Continuum Health Partners, Inc.
Lee Burns, PCN
Emergency Medical Services
NYS Department of Health
Andrew J. Chen, CHE
Assistant Vice President
Hospital for Joint Diseases Orthopedic Institute
Edward E. Conway Jr., M.D., M.S.
Professor and Chairman
Pediatrician-in-Chief
Milton and Bernice Stern Department of Pediatrics
Chief Division of Pediatric Critical Care
Beth Israel Medical Center
Rose Marie Davis, RN
Emergency Medicine
Manhattan VA
VA New York Harbor Healthcare System
Donald J. Decker, CSW, CASAC
Hospital Coordinator
Office of Mental Health Disaster Preparedness
and Response
NYC Department of Health & Mental Hygiene
Bernard P. Dreyer, MD
Associate Chairman of Pediatrics
New York University School of Medicine
Chief of Pediatrics
Bellevue Hospital Center
Judith Faust
Director
Bioterrorism Hospital Preparedness Program
New York State Department of Health
Elliot M. Friedman, MD FAAP PEN
Assoc. Director, Emergency Services
Director, Pediatric Emergency Services
Jamaica Hospital Medical Center
Franklin Fleming, RN
Emergency Medicine
Manhattan VA
VA New York Harbor Healthcare System
Jessica Foltin, MD, FAAP
Director
Pediatric Emergency and Transport Medicine
New York University School of Medicine
Lorraine Giordano, MD, FACEP
Medical Director
NYC Health & Hospital Corporation
NYC Office of Emergency Management
Margaret Graham
Consortium on Preparedness
New York University School of Medicine
Hyacinth Hamilton-Gayle, RN MSN, PNP
Director of Nursing, WCH
Brookdale Hospital Medical Center
Dennis Heon
Pediatric Emergency Medicine
Bellevue Hospital Center
Jeffrey Hom, MD, MPH
Department of Emergency Medicine
Assistant Professor
SUNY-Downstate/Kings County Hospital
Lewis Kohl, MD
Director of Emergency Medicine
Long Island College Hospital
Danielle Laraque, MD, FAAP
Professor of Pediatrics
Mount Sinai School of Medicine
Lori Legano, MD
Assistant Director Child Protective Services
Assistant Professor of Pediatrics
Bellevue Hospital Center
Andrea O’Neill, MD
Trauma Coordinator Department of Surgery
Bellevue Hospital Center
Joseph Marcellino
NYC Office of Emergency Management
David Markenson, MD, FAAP, EMT-P
Director Program for Pediatric Preparedness
Mailman School of Public Health
Columbia University
Director of Pediatric Intensive Care
Flushing Hospital Medical Center
Diorelly Marquez, RN
Emergency Medicine
Manhattan VA
VA New York Harbor Healthcare System
Gloria Mattera
Director
Department of Child Life and Development Services
Bellevue Hospital Center
Margaret McHugh, M.D., MPH
Clinical Associate Professor Pediatrics
NYU School of Medicine
Director Adolescent Ambulatory Services
Bellevue Hospital Center
Shelly Mazin
Director of Safety
Bellevue Hospital Center
Chantal Michel, RN, CEN
Associate Director Emergency Department
Woodhull Medical and Mental Health Center
Marurizio A. Miglietta, DO
Assistant Professor of Surgery
Department of Surgery
Bellevue Hospital Center
Shari L. Platt, MD
Director, Division of Pediatric Emergency Medicine
Komansky Center for Children’s Health
New York Presbyterian Hospital –
Weill Cornell Medical Center
David Roccaforte, MD
Assistant Professor Department of Anesthesiology
New York University School of Medicine
Co-Director Surgical Intensive Care Unit
Bellevue Hospital Center
David Rohland, PhD
Director Psychiatry
Manhattan VA
VA New York Harbor Healthcare System
Diane Rosenstein
Social Work Supervisor
NYU Medical Center
Mort Rubenstein
Deputy ACOS
Mental Health New York
VA New York Harbor Healthcare System
Ashraf Salem, MD
Assistant Disaster Coordinator
SUNY Downstate Medical Center
Raul R. Silva, M.D.
Deputy Director if the Division of Child and Adolescent Psychiatry
Associate Professor of Psychiatry
NYU Medical Center
Dennis Sklenar, LCSW
Senior Social Worker
Social Work Department
NYU Medical Center
Lewis Soloff, MD
Senior Medical Coordinator
Bioterrorism Hospital Preparedness Program
NYC Department of Health & Mental Hygiene
Sunil Sachdeva, MD
Assistant Director Pediatric Emergency Medicine
Long Island College Hospital
Angela Tangredi, MD
Department of Emergency Medicine
St. Luke’s Hospital
Continuum Health Partners
Marsha Treiber, MPS
Pediatric Emergency Medicine
Bellevue Hospital Center
Michael G. Tunik, M.D.
Associate Professor
Pediatrics Emergency Medicine
Bellevue Hospital Center
Michael Ushay, MD
Director of Pediatric Critical Care Fellowship
Schnnider’s Children’s Hospital
Doris Varlese
Associate General Counsel
Greater New York Hospital Association
Peter Ventri
Director of Staff Development and Training
Kingsbrook Psychiatric Center
Maurice Wright, MD
Chairman Emergency Medicine
Woodhull Medical & Mental Health Center
Table of Contents
General Recommendations of the PDAG Task Force
- General Guidelines
- Patient Tracking Options
- Pediatric Patient Tracking – The Accompanied Child
- Pediatric Patient Tracking – The Displaced or Unaccompanied Child
- Protocol to Rapidly Identify and Protect Displaced Children
- Child ID Survey Form
- Setting Up a Pediatric Safe Area
- Pediatric Area Safe Checklist
- Job Action Sheet: Pediatric Safe Area Coordinator
- Pediatric Safe Area Registry Sheet
Section 2. Dietary Needs of Children
- General Guidelines
- Food Supply Recommendations for Healthy Children
- Dietary Recommendations for Special Needs Children
- Sample Pediatric Disaster Menus
- General Guidelines
- Transfer Considerations for Hospitals without PICU
- Planning Scenario
- Emergency Department Surge Considerations and In–Patient Bed Assignments
- Non-Trauma Hospitals with a PICU
- Hospitals with a Pediatric Service but without a PICU
- Hospitals without Pediatric Services
Section 4. Equipment for Pediatric Disasters
- Table: Minimal Pediatric Equipment Recommendations for Emergency Departments
Section 5. Training for the Care of the Pediatric Population during a disaster
- General Guidelines
- Training Recommendations:
- Non-Trauma Hospitals with a PICU
- Hospitals with a Pediatric Service but without a PICU
- Hospitals without Pediatric Services
- Table of Training Recommendations
- List of Additional Disaster and Emergency Courses
Section 6. Transportation of Pediatrics during Disasters
- General Guidelines
- Transport of Pediatric Patient within the Hospital
- Transport of Pediatric Patient from Hospital to Other Facilities
- Table 6.1: Appropriate Use and Type of Car Seats
Section 7. Staffing Recommendations for Pediatrics in Disasters
- General Guidelines
- Planning: Survey Staff for Pediatric Experiences
- Mitigation: Create Pediatric Leadership Positions
- Physician Coordinator for Pediatric Emergency Care in a Disaster
- Nursing Coordinator for Pediatric Emergency Care in a Disaster
- Response: Staffing for a Coordinated and Comprehensive Disaster Plan
- Sample HEICS Job Action Sheets
- Pediatric Services Unit Leader
- Pediatric Logistics Unit Leader
Section 8. Decontamination of the Pediatric Patient
- General Guidelines for Decontamination
- Decontamination Recommendations Based on Age of Child
- Model Decontamination Algorithm
- References
Section 9. Pharmacy Needs of Pediatrics in Disasters
- General Guidelines for Pediatric Pharmacy Needs
- Pharmacy Inventory (Pediatrics)
- Drug Preparation and Dosing:
- Table 8.1 Doxycycline suspension
- Table 8.2 Sodium nitrate
- Table 8.3 Oseltamvir
- Table 8.4 Potassium Iodide Solution
- Table 8.5 ThyroShield Dosing Recommendations
- Table 8.6 Mark-1 Kit Use in Pediatrics – NYC Protocol
- References and Web Sites
Section 10. Psychosocial Needs of Children during Disasters
- General Guidelines for Psychosocial Needs of Children
- Helping Children in a Medical Setting: Development Specific Guidelines
- How Children React to a Disaster
- Helpful Hints to Assist Children
- When to Consult a Mental Health Professional
- Legal Considerations
- Cultural Differences about Death and Dying
- Obtaining Mental Health Services in the Community
- Fact Sheet: After a Disaster: A Guide for Parents and Care–Givers
- On–line Resources for Pediatric Psychosocial Issues
Section 11. Pediatric Infection Control Considerations
- General Guidelines for Infection Control for Children
- Infection Control Measures for Exposed/Asymptomatic Children
- Infection Control Measures for Exposed/Symptomatic Children
- Co-horting of Children in a Hospital Setting
- Environmental Measures for Pediatric Units
- Staff Child Ratio and Group size Indicator
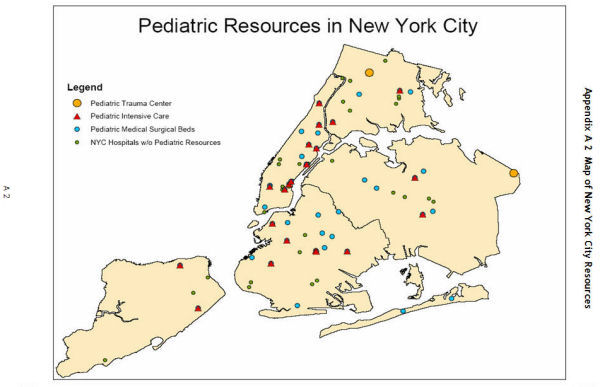
Appendix A: New York City Specific Resources
- Table of Hospitals with Pediatric Intensive Care Unit Beds
- Map of New York City Pediatric Resources
CBPP Pediatric Task Force Initiative:
Hospital Guidelines for Pediatrics in Disasters
Draft for Public Comment
Introduction
During of a mass casualty or terrorist event, it is recognized that all hospitals, even those that are not pediatric trauma centers or specialized pediatric hospitals, might receive critically ill or injured pediatric patients. Additionally, it is acknowledged by the health care community of New York City that there has been limited attention to the specific needs of the pediatric population and their families in disaster response preparation. This planning gap has been recognized by the New York City Department of Health and Mental Hygiene (DOHMH ). The Department in turn tasked the Centers for Bioterrorism Preparedness Planning (CBPP)1 to assist the DOHMH in preparing NYC hospitals for the needs of this special population.
Two CBPPs, the Central Brooklyn Center for Bioterrorism Preparedness Planning and the New York Center for Terrorism/Casualty Preparedness, have been the institutional leaders in this initiative. The goal of their efforts is to provide hospitals, especially those that do not normally admit Children, or have no Pediatric Intensive Care Services or Obstetrical/Newborn services, some useful, proactive planning strategies and tools for providing protection, treatment, and acute care for pediatric patients during a disaster. The following hospital guidelines and recommendations for Children in disasters are the first examples of the on-going work of the CBPP Pediatric Task Force.
Structure of CBPP Pediatric Task Force
The CBPP Pediatric Task Force is comprised of pediatric emergency medicine and critical care physicians, social workers, emergency managers, and others with specific training, interest, and experience in pediatric specialty care. The task force met bimonthly during 2005 and 2006 to discuss hospital mass casualty preparedness planning and necessary pediatric-specific care considerations. The role of the Pediatric Task Force has been to provide a pediatric disaster preparedness focus and expert multi-disciplinary advice to hospitals to prepare for pediatric care considerations in the event of a disaster.
This group met and developed a mission statement at the beginning of 2005:
"We, the CBPP Pediatric Task Force, under the guidance/auspices of the NYC DOHMH Pediatric Disaster Advisory Group, in an effort to safe-guard the pediatric population, will advise the Healthcare community and NYC agencies on the appropriate planning necessary to ensure the proper care of Children and their families in the event of a disaster."
Clear specific outcomes for 2005-2006 project years were developed and agreed on by the entire task force with additional input and approval from DOHMH . It was the plan of the group to not have too large an initial set of goals so that success could be achieved. The CBPP Pediatric Task Force has been slated by the NYC DOHMH to continue for an additional year, refining and adding to the “Hospital Guidelines for Pediatrics in Disasters,” and addressing other regional pediatric health issues in the future.
Focus of Guidelines
At the first meeting of the CBPP Task Force, three groupings of “hospitals of concern” were identified: Hospitals without Pediatric Services, Hospitals without Pediatric Intensive Care Services, and Hospitals without Pediatric Trauma Services. Additionally, ten section topics related to pediatric disaster preparedness were selected:
- Staffing
- Space and Equipment Needs
- Security
- Transportation Needs
- Training Recommendations
- Psychosocial / Ethical Considerations
- Pediatric Dietary Needs
- Decontamination of Children
- Pharmaceutical Planning
- Pediatric Infection Control Considerations
Although these ten topics are not comprehensive in regard to all aspects of planning for the special needs of the pediatric population, creating some useful expert-reviewed guidance documents and planning tools in these areas would greatly reduce the amount of development and planning time for each individual hospital.
Individual task members contributed draft documents in the areas of interest and expertise, including literature searches for each area, and reported back to the group. In the area of Pediatric Disaster Preparedness it was discovered that literature existed, yet most of what was found gave only generalized recommendations. Contributors have attempted to develop user-friendly “how to” documents with clear and specific suggestions. Many of the documents were created based on the group member’s own hospital-based experience. Others were adapted from available resources. All drafts have been initially reviewed by task force members with several iterations being created.
Review Process
All documents created by the task force have had additional review by the NYC DOHMH Pediatric Disaster Advisory Group (PDAG ). This advisory group was established to support the efforts of the NYC DOHMH pediatric preparedness and response planning efforts for New York City. PDAG members include pediatric experts from multiple academic and community hospitals in the New York City metropolitan region, as well as representatives from city and state agencies. The almost 50 members of PDAG reviewed and contributed comments on the following documents, and also made suggested to topics to be addressed by the CBPP Pediatric Task Force and the NYC DOHMH in future.
General Recommendations of the CBPP Task Force
Force Concerning Hospital Planning for Pediatrics during a Disaster
- All Hospitals Should Plan for Pediatric Patients Arriving during a Disaster
The following document addresses the issues surrounding pediatric emergency care during a disaster. It is presented under the supposition that all hospitals need to recognize the potential for receiving pediatric patients during a disaster and appropriately plan for pediatric mass casualty care. In a disaster event, the following may occur:
- Pediatric patients might present to ANY hospital
- Critically ill pediatric patients might present to ANY hospital
- Transfer of patients to specialized hospitals might not be feasible
Therefore, during disasters all hospitals and all providers must be prepared to deliver care to pediatric patients. During the 9/11 terrorist event, nearly 100 different hospital received patients. While most of these patients walked, ran, took buses, taxis or boats, the minority waited to be transported by ambulance. Self-evacuating pediatric victims and their care givers will go to the nearest hospital, the most convenient hospital, or the hospital they are most familiar with regardless of the capabilities of that hospital for specialty or pediatric care.
All hospitals, even those that are not pediatric trauma centers or specialized pediatric hospitals, might receive critically ill or injured Children in a mass casualty or disaster event. Pediatric patients may initially be brought to the nearest centers, as ambulances attempt to expedite their return to the disaster scene to maximize the care of patients. Even after on-scene triage is established, severely injured Children may be brought to the nearest medical centers because the patient is simply too unstable to survive a longer transport time. Additionally, due to traffic congestion, unsafe conditions, or lack of appropriate vehicles, ambulances may be initially unable to perform more distant transportation.
Each hospital, even hospitals that do not routinely provide pediatric services, needs to plan for the possibility that pediatric patients arriving at their hospital during a disaster might require emergency evaluation, critical care, surgical services, inpatient care, and psychosocial support and should be prepared to offer these services accordingly.
- Plan for Transport of Pediatric Patients
Hospital centers should address the possibility that the number of pediatric patients requiring admissions might exceed their normal patient capacity or expertise of hospital staff. For those centers without speciality pediatric services, transfer of patients to a center with specialty pediatric services may be necessary. Hospitals should establish relationships with appropriate hospital facilities that do admit pediatric and obstetrical patients, and a Stabilize and Transfer Agreement should be developed with those facilities.
Consideration for agreements should go beyond traditional network relationships and should include geographical proximity due to the unpredictability of traffic obstructions during the acute phase of a disaster.
- Plan for Pediatric In–Patient Care if Transport is Delayed
During the first 24 to 48 hours of a disaster involving much of the region, transfer might be difficult or impossible due to local conditions, lack of transport vehicles and personnel, or lack of capacity at pediatric resource hospitals. Therefore, all hospitals must be prepared to provide emergent pediatric care and In–Patient admission, even for critically injured pediatric patients until such time that safe transport can be arranged. For hospitals without pediatric intensivists or pediatric trauma surgeons, it is recommended that relationships be developed with pediatric intensive care specialists and pediatric trauma surgeons at outside hospitals to provide, at the minimum, telephone consultations or support for admitting physicians.
- Survey Staffing for Pediatric Expertise
Physicians, nurses, Social Workers, and other staff in the emergency department (ED ) and In–Patient areas at a given hospital must have the necessary skill, knowledge and training to provide timely efficient care in the event of a disaster. Many levels of staffing are required including the ability to provide emergency evaluation and treatment of Children who may be brought to the ED . Yet, not every hospital has a full complement of pediatric specialists and nurses.
It is recommended that individual hospitals and networks survey their own staff and admitting physicians to develop a database of personnel with pediatric experience and training. For example, the Emergency Department physicians may have considerable experience with Children; Anesthesiologists and/or Otolaryngologists may be knowledgeable about intubations of Children.
- Appoint a Pediatric Physician Coordinator and a Pediatric Nursing Coordinator
It is recommended to appoint both a Physician Coordinator for Pediatrics, and a Nursing Coordinator for Pediatrics. These coordinators should serve as a liaison between different internal and external hospital pediatric care committees, provide assistance and support for education of hospital providers affiliated with the ED and assist in the development and use of pediatric hospital protocols and procedures. It is envisioned that these positions would advocate for Children’s needs during planning and responding to a disaster involving Children.
- Increase Pediatric and Disaster Training
Increased numbers of medical staff should be trained to provide appropriate basic pediatric emergency care in Advanced Cardiac Life Support (ACLS), Advanced Trauma Life Support (ATLS), Advanced Pediatric Life Support (APLS), basic disaster education and pediatric disaster drills. Additionally, there are training courses provided by the American Heart Association, called Neonatal Advanced Life Support (NALS) and Pediatric Advanced Life Support (PALS), of which “abridged” versions may be taught to hospital staff on an ongoing basis. Updates and re-certifications should be arranged as well. New versions of Chemical, Biological, Radiological, Nuclear, and Explosive (CBRNE) Hazardous Materials Classes should include pediatrics and the specific needs of Children and their families during a disaster involving hazardous materials.
Pediatric Security Issues during a Disaster
Draft for Public Comment
Purpose:
- Previous literature regarding the security of the pediatric population primarily addressed preventing infant abductions. The recent Gulf Coast hurricanes of 2005 highlighted the importance of this critical need in the care of the pediatric population. The following recommendations for pediatric security during a disasters is intended to assist planning for the needs of all pediatric patients presenting to any hospital during a disaster. The recommendations included in this section focus primarily on pediatric patient/visitor tracking and creating pediatric safe areas.
Section Contents:
- General Guidelines
- Pediatric Tracking Option
- Tracking options for both the accompanied and the unaccompanied or displaced Child are discussed
- Protocol to Rapidly Identify and Protect Displaced Children
- Hospital protocol modified from the CDC Health Advisory, “Instructions for Identifying and Protection Displaced Children,” Sept. 28, 2005
- Child ID Survey Form
- Sample survey form utilized in the Protocol to Rapidly Identify and Protect Displaced Children
- Setting Up a Pediatric Safe Area (PSA)
- Recommendations for establishing a supervised area within the hospital to safely cohort unaccompanied Children during a disaster
- Pediatric Safe Area Checklist
- Steps useful to create a Pediatric Safe Area
- Job Action Sheet: Pediatric Safe Area Coordinator
- JAS for supervising staff for the Pediatric Safe Area
- Pediatric Safe Area Registry Sheet
- Sample registry form for the Pediatric Safe Area, utilized to assist staff to document location and final disposition of Children
General Guidelines:
All hospitals responding to a disaster are advised to:
- Develop a Pediatric Tracking System that addresses both the accompanied and unaccompanied Child.
- Develop a protocol to rapidly identify and protect displaced Children.
- Create a Child ID document to record any key identifying information about Children or use in later tracking or reunion with caregivers.
- Create Pediatric Safe Areas that will serve as a holding area for uninjured, displaced or released Children awaiting adult caregivers. A Pediatric Safe Area Checklist has been provided to assist in the establishment of such areas.
- Identify a Pediatric Safe Area (PSA) Coordinator who will assume the responsibility of setting up and supervising the pediatric safe area in the event of a disaster. Included in this section is a Sample Job Action Sheet which outlines the PSA Coordinator position.
- Create and use a Pediatric Safe Area registry sheet to document activity, such as transfer status, location, and final disposition, regarding the Child.
Pediatric Patient Tracking
The issue of pediatric patient tracking has historically been restricted to maternity and pediatric wards. Much of the literature refers to the cases of infant security and the reduction of pediatric patient abductions from various hospital wards. There are specific measures discussed that can be taken to prevent the abduction of pediatric patients, such as the use of identification bands for the pediatric patient. However, there is no discussion of identification for the pediatric visitor in a hospital.
Hospitals have historically served as safe havens for displaced persons during a disaster. During the August 2003 Blackout, many members of the NYC community came to hospitals as secure places known to have functioning generators and supplying light, safety, and nourishment. Abandoned Children are also often brought first to a hospital emergency department for evaluation. During a disaster, hospitals may again serve as safe havens and may find themselves host to displaced and unaccompanied Children. As a recent example, Hurricane Katrina and the ensuing floods and chaos caused over 3,000 Children to be displaced throughout the United States1. These displaced Children, if unaccompanied, are at special risk for maltreatment, neglect, exploitation, and subsequent psychological trauma. Hospitals and medical clinics will therefore need to be especially alert to the safety and mental health issues of these Children.
The focus of this document is to raise the level of awareness regarding the issue of the pediatric population and security issues during an emergency or incident that would require a Child to go to a hospital. Hospitals, especially those that do not routinely take care of the pediatric population, need to pay special attention to the specific security needs of this group and take the necessary precautions to ensure proper care of these individuals while they are in the hospital.
Patient Tracking – the Accompanied Child in a Disaster
There are two populations of accompanied Children during a disaster that should be addressed:
- The pediatric patient who is actually a patient of the hospital as a result of the disaster and who may become separated from the responsible adult; for example, if the responsible adult is also a patient.
- The pediatric visitor who is not a patient of the hospital but who may be accompanying an adult person who is a patient; for example, a critical adult patient who was caring for a minor at the time of the disaster or event.
A possible solution to tracking these persons is to use a system of identification bands for the minors and corresponding responsible adults that are distributed as soon as these individuals make contact with ED area. Care must be taken to quickly and correctly place bands or other identification devices on both parties.
Special attention needs to be taken to ensure that this measure is completed as soon as possible at the entry point to the hospital to reduce the possibility of human error during the matching and placing of the bands.
There are hospital policies in place for the tracking of minors from pediatric and maternity wards. These identification bands are used on all patients as they enter the hospital. The specific concern raised here is minors accompanying the adults during a disaster-level event who could easily be lost during the chaos of a disaster event.
The identification bands used should include the following information which will be useful in maintaining a tight link between pediatric patient/ visitor and adult:
- Name of pediatric patient/ visitor + DOB
- Name of adult + DOB
- Admission date of adult
- Admission date of pediatric patient
- Date of visit of pediatric visitor
In addition, a more sophisticated approach to tracking could be implemented by the use of bar coded bracelets as identifiers that can be affixed to the pediatric patient / visitor and to the adult at the time of entry to ED or other entry point of the hospital. In this manner, the same bar code is assigned to the adult and the pediatric patient/ visitor (s) with the adult.
For further information, hospitals may also review the infant abduction protocols in place at their facility.
Patient Tracking – the Displaced or Unaccompanied Child in a Disaster
Rapid identification and protection of displaced Children (less than 18 years) is imperative in order to reduce the potential for maltreatment, neglect, exploitation, and emotional injury. A critical aspect of pediatric disaster response is effectively addressing the needs of Children who have been displaced from their families and legal guardians. The separation of Children from significant others is a recognized factor influencing the psychological responses of Children after a disaster.
All hospitals, medical clinics, and shelters providing care to Child survivors of disasters should immediately implement appropriate Child-safety measures in direct response to this crisis. Initiatives such as “Operation Child ID” implemented in Camp Gruber Oklahoma after Hurricane Katrina in 2005 have provided a rapid, systematic protocol for successfully identifying and protecting displaced Children. The CDC has reviewed this protocol and considers it to be a useful resource to share with its partners to promote a safer and healthier environment for displaced Children in shelters1. The following protocol on page 1-5 has been adapted to address displaced Children during disasters in New York City:
- CDC Health Advisory, “Instructions for Identifying and Protecting Displaced Children.” Sept. 28, 2005.
Protocol to Rapidly Identify and Protect Displaced Children
- Survey all Children in your hospital, medical clinic, or shelter to identify Children who are not accompanied by an adult; these Children have a high probability of being listed as missing by family members. Find out where they are sleeping/being held and the name and age of person(s) who is/are supervising them, if available. A sample survey form for identifying displaced Child is attached.
- Place a hospital-style identification bracelet (or, ideally, a picture identification card) on the Child and a matching one on the supervising adult(s), if such an adult is available. Check frequently to make sure that the wrist band matches that of the adult(s) seen with the Child in the hospital or shelter. If there is no supervising adult, the Child should be taken to the hospital’s pre-determined Pediatric Safe Area (see following pages) where he/she can be appropriately cared for until a safe disposition or reunification can be made.
- The names of all Children identified through the survey as not being with their legal guardians or who are unaccompanied should be considered at high-risk and immediately reported to the hospital’s emergency operations center. Additional reporting should also be made to the National Center for Missing and Exploited Children (NCMEC) at 1-888-544-5475. The NCMEC can then cross-check them with the names of Children who have been reported missing.
- After the “high risk” Children have been reported, a complete list of all Children names in the hospital, clinic or shelter should be sent to NYS Hospital Emergency Resource Database System (HERDS) if activated and the information is requested. The complete list should also be sent the NCMEC in case adults and/or Children have provided incorrect information about their relationship and status.
- Unaccompanied Children and those who are not with their legal guardians should undergo a social and health screening taking into consideration an assessment of the relationship between the Child and accompanying adult, ideally performed by a physician with pediatric experience.
- If NYS DOH, another NYC agency, or NCMEC informs you that the Child has been reported as missing, locate the Child and facilitate reunification of the Child and his/her legal guardian.
- CDC Health Advisory, “Instructions for Identifying and Protecting Displaced Children.” Sept. 28, 2005.
Child ID Survey
| Name: | |
| Hospital # | |
| Age: | Months/Years |
| DOB | |
| Gender: | Male Female |
| Is the Child currently accompanied by a supervising adult? | Yes No |
| Name of currently the supervising adult? | Age |
| Is this person a Parent? | Yes No |
| A Grandparent? | Yes No |
| Is this parent the usual guardian? | Yes No |
| Was the Child living with this person before the disaster? | Yes No |
| Does the supervising adult have any proof of legal guardianship or relationship to Child? | Yes No |
| If Yes, please describe or attach a copy: | |
| If the adult(s) is not a Parent or Grandparent, what is the relationship to this Child? | |
| Aunt/Uncle | Age |
| Sibling | Age |
| Friend< | Age |
| Other (next-of-kin, teacher) | Age |
| Was the Child treated for illness or have an injury? | Yes No |
| If yes, please describe: | |
| Was the Child admitted to the hospital? | Yes No |
| If Yes, give room or location | |
| If No, give location or address where Child is currently (lobby, Pediatric Safe Area, sent to shelter, etc.) | |
| Does this Child have a history of medical problems? | Yes No |
| If yes, please list: | |
| Does this Child or family members have special needs? | Yes No |
| If yes, please list: | |
Pediatric Safe Areas
Supervised areas should also be created to cohort all unaccompanied pediatric visitors or unaccompanied released pediatric patients in one central and safe location. This central location will need to be pre-assigned and secured to ensure that minors can not leave the area without appropriate escorts. Security personnel or other responsible staff will need to be trained to supervise and assist pediatric visitors who may be frightened or who have other mental health issues as a result of being involved in a disaster and separated from family members.
Included in this section are three forms that may be helpful for hospital planning required for a Pediatric Safe Area. These forms include:
- Pediatric Safe Area Checklist. This form was adapted from the Chicago Department of Health, and outlines recommended steps to ensure that the Pediatric Safe Area is appropriately set-up to receive Children.
- Pediatric Safe Area Coordinator Job Action Sheet (JAS). Created for the staff coordinating these pediatric safe areas. By having a JAS, staff can readily review what steps need to be taken to prepare for the possible influx of pediatric patients. See JAS at the end of this chapter.
- Pediatric Safe Area Register. This is a sample of a form that could potentially be used in the Pediatric Safe Area to monitor the arrival and departure of Children. A copy of this register should be made available to the hospital EOC on a frequent basis.
Pediatric Safe Area Checklist
| Yes | No | Item |
|---|---|---|
| Needle boxes are at least 48 inches off the floor? | ||
| Do the windows open? | ||
| Are the windows locked? | ||
| Do you have window guards? | ||
| Can you contain Children in this area (consider stairwells, elevators, doors)? | ||
| Do you have distractions for the Children (age and gender appropriate videos, games, toys)? | ||
| Poison-proof the area (cleaning supplies, Hemoccult developer, choking hazards, cords should be removed or locked) | ||
| Are your med carts and supply carts locked? | ||
| Do you need to create separate areas for various age groups? | ||
| Have you conducted drills of the plans for this area with all relevant departments? | ||
| Do you have a plan for security for the unit? | ||
| Do you have a plan to identify the Children? | ||
| Do you have a plan for assessing mental health needs of these Children? | ||
| Are there any fans or heaters in use? Are they safe? | ||
| Do you have an onsite or nearby daycare? Could they help you? | ||
| Do you have enough staff to supervise the number of Children (Younger Children will require more staff)? | ||
| Do you have a sign-in, sign-out sheet for all Children and adults who enter the area? | ||
| Will Children need to be escorted away from safe area to bathrooms? | ||
| Are age appropriate snacks available for Children? |
Sample Job Action Sheet
Pediatric Safe Area (PSA) Coordinator
You report to:_______________________(Pediatric Services Unit Leader)
Command Center___________________________________________________
Mission:
To ensure that the pediatric safe area is properly staffed and stocked for implementation during an emergency, and to insure the safety of Children requiring the PSA until an appropriate disposition can be made.
Immediate:
- Receive appointment from Pediatric Services Unit Leader
- Read this entire job action sheet
- Obtain briefing from Pediatric Services Unit Leader
- Ascertain that the pre–designated pediatric safe area is available
- If not immediately available, take appropriate measures to make the area available as soon as possible
- Gather information about how many pediatric persons may present to the area
- Make sure that enough staff is available for PSA
- Make sure that enough security staff is available for PSA
- Make sure that there is adequate communication in PSA
- Make sure that there is a sign in/out log for PSA
- Make sure that all items in PSA checklist have been met; if there are any deficiencies, address them as soon as possible and report them the PSUL
Intermediate:
- Ascertain the need for ongoing staff for PSA
- Maintain registry of Children in PSA as they arrive or are released to appropriate adult
- Determine estimated length of time for the expected operational period of PSA
- Maintain communication with Pediatric Services Unit Leader for planning needs
- Determine if there are any medical or non-medical needs specifically needed by pediatric persons in PSA
- Prepare an informational session for the pediatrics persons in the PSA
- Prepare to make arrangements for sleeping capacities if needed
- Ascertain if there will be any additional needs required for this event (volunteers, staff, security, and equipment)
- Make sure that pediatric persons have the appropriate resources (food, water, medications, age-appropriate reading materials) and entertainment for their stay
- Report frequently to Pediatric Services Unit Leader concerning status of PSA
Extended:
- Make sure that PSA staff have enough breaks, water, and food during their working periods
- Coordinate with Psychological Support for ongoing evaluations of mental health of volunteers and pediatric persons in case of need for psychosocial resources
- Document all action/decisions with a copy sent to the Pediatric Services Unit Leader
- Other concerns: _____________________________________________________
Pediatric Safe Area Registry Sheet
| # | Name of Child | Age | Arrival Time | Discharge Time | Disposition | Responsible Adult Name | Responsible Adult Signature | Contact Phone Number |
|---|---|---|---|---|---|---|---|---|
| 1 | ||||||||
| 2 | ||||||||
| 3 | ||||||||
| 4 | ||||||||
| 5 | ||||||||
| 6 | ||||||||
| 7 | ||||||||
| 8 | ||||||||
| 9 | ||||||||
| 10 | ||||||||
| 11 | ||||||||
| 12 | ||||||||
| 13 | ||||||||
| 14 | ||||||||
| 15 | ||||||||
| 16 | ||||||||
| 17 | ||||||||
| Disposition: Admit to Hospital (A) Discharged to Parent (D-P) Discharged to relative (D-R) Discharged to Other (D-O) Social Services Placement (SS) Police (NYPD) Responsible Adult: Adult responsible for Child at time of discharge. PSA Coordinator should determine if Child can be discharged to this adult based on hospital policy. | ||||||||
Section 2. Dietary Needs of Children
Pediatric Dietary Needs
Draft for Public Comment
Purpose:
In order to adequately prepare for an influx of pediatric patients that may result from a disaster involving Children, hospitals must also consider the requirements for providing food to this population while they are patients or visitors in the facility. The Pediatric Dietary section provides nutritional guidelines for hospitals that do not typically provide pediatric In–Patient services.
The recommendations in this section include: pediatric dietary recommendations for healthy Children and Children with special needs, and sample disaster menus for Children including those that have special dietary needs. The menus focus on foods that require little to no preparation and are both easy and inexpensive to store.
Section Contents:
- General Guidelines
- Table 2.1 Pediatric Dietary Recommendations
- Healthy Child
- Special Needs Child
- Diabetic Child
- Sample Pediatric Disaster Menu
- A sample diet for pediatric patients listing foods that require a minimal amount of preparation or power supply to maintain food temperatures
General Guidelines:
The CBPP Pediatric Task Force recommends that hospitals maintain a 5-day food supply for use during an emergency. It is also recommended that each institution maintain Memorandums of Understanding (MOUs) with nearby stores, for example: local groceries, pharmacies, and medical supply stores, to provide the hospital with immediate delivery and additional supplies.
The nutritional supplies recommended for both healthy Children and those with special dietary needs are listed in Table 2.1 Pediatric Dietary Recommendations found on the following pages.
| Table 2.1 Pediatric Dietary Recommendations | ||||
|---|---|---|---|---|
| 0-6 months | 6 months to 1 year | 1 to 2 years | 2 years and above | |
| Healthy Children | These Children are breast fed or formula fed by bottle only. Comments: Some breast fed Children may not immediately take bottle-feeding.Continue to feed; eventually the Child will feed from the bottle. Recommendation: Ready-to-feed formula is preferred since it is immediately ready for use and requires no refrigeration or preparation. However, powdered baby formula may be used as well. Powdered formula will have a longer shelf life. |
6-9 months – baby cereal, jarred baby food or mashed table food is appropriate – along with formula or breast milk 9-12 months – soft, bite sized pieces of foods, i.e. vegetables, mashed potatoes, and meats – along with formula or breast milk |
This age group eats table food. Young Children will need soft bite sized foods. Avoid foods that can cause choking such as hot dogs, grapes, chunks of meat unless cut in pea size pieces Hydration: Water, Pedialyte See Attached Sample Menu |
This age group eats table food. Young Children will need finger foods. Avoid foods that can cause choking such as hot dogs, grapes, for youngest Children. Hydration: Water, Pedialyte See Attached Sample Menu |
| Children With Special Needs | Patients with feeding tubes: There are (3) types of tube feeding: Nasogastric (N/G), Orogastric, and Gastrostomy (G/T). The first two are used for acute patients; the third is used for chronic patients. N/G and O/G Tube: Used for both nasal and orogastric feedings and are temporary measures, mostly used in Pediatric Emergency Rooms or Pediatric In–Patients areas for acute feeding issues, gastric decompression, and/or delivery of oral medications such as activated charcoal. G/T Tube: Used with a 60cc syringe, catheter tip and is used with a bolus continuous feed or pump. Infants (0-12months): Infant formula should be used through the tube. 12 months to18 years of age: Pediatric formulas should be used, i.e. Resource Just for Kids, PediaSure or Nutren Jr. For adolescents, based on clinical judgment adult enteral product may be appropriate. Hydration: Tap or bottled water.
|
|||
| Diabetic Children | The nutritional needs of this group will be determined by the patient’s body weight and insulin requirements. Recommendation: Patients may require between meal snacks to control blood glucose. |
|||
References: ADA Manual of Clinical Dietetics. (2000), Sixth Edition.
Sample Pediatric Disaster Menu
The following sample diet for pediatric patients lists foods that require the minimal amount of preparation or power supply to maintain temperatures.
| Day 1 | Day 2 | Day 3 | |
|---|---|---|---|
| Breakfast | Breakfast | Breakfast | |
| 0-6 months | Regular or Soy Formula | Regular or Soy Formula | Regular or Soy Formula |
| 6 months - 1 yr. | Baby Cereal | Baby Cereal | Baby Cereal |
| Jarred Baby Fruit | Jarred Baby Fruit | Jarred Baby Fruit | |
| Regular or Soy Formula | Regular or Soy Formula | Regular or Soy Formula | |
| 1 yr. and above | Cheerios (or Substitute) | Cheerios (or Substitute) | Cheerios (or Substitute) |
| Parmalat (1-2 years) | Parmalat (1-2 years) | Parmalat (1-2 years) | |
| Powdered Milk (> 2 years) | Powdered Milk (> 2 years) | Powdered Milk (> 2 years) | |
| Diced Canned Fruit | Diced Canned Fruit | Diced Canned Fruit | |
| Lunch | Lunch | Lunch | |
| 0-6 months | Regular or Soy Formula | Regular or Soy Formula | Regular or Soy Formula |
| 6 months - 1 yr. | Jarred Baby Meat | Jarred Baby Meat | Jarred Baby Meat |
| Jarred Baby Vegetable | Jarred Baby Vegetable | Jarred Baby Vegetable | |
| Jarred Baby Fruit | Jarred Baby Fruit | Jarred Baby Fruit | |
| Regular or Soy Formula | Regular or Soy Formula | Regular or Soy Formula | |
| 1 yr. - 2 yrs. | Cream Cheese/Jelly Sandwich | Macaroni and cheese | Cheese Wiz© |
| Jarred Baby Vegetable | Jarred Baby Vegetable | Jarred Baby Vegetable | |
| Diced Peaches | Diced Pears | Diced Fruit Cocktail | |
| Bread/Crackers | Bread/Crackers | Bread/Crackers | |
| Parmalat | Parmalat | Parmalat | |
| 2 yrs. plus | Cream Cheese/Jelly Sandwich | Macaroni and cheese | Peanut Butter/Jelly Sandwich* |
| Diced Peaches | Diced Pears | Diced Fruit Cocktail | |
| Graham Crackers | Graham Crackers | Graham Crackers | |
| Powdered Milk | Powdered Milk | Powdered Milk | |
| Dinner | Dinner | Dinner | |
| 0-6 months | Regular or Soy Formula | Regular or Soy Formula | Regular or Soy Formula |
| 6 months - 1 yr. | Jarred Baby Meat | Jarred Baby Meat | Jarred Baby Meat |
| Jarred Baby Vegetable | Jarred Baby Vegetable | Jarred Baby Vegetable | |
| Jarred Baby Fruit | Jarred Baby Fruit | Jarred Baby Fruit | |
| Regular or Soy Formula | Regular or Soy Formula | Regular or Soy Formula | |
| 1 yr. - 2 yrs. | Cheese slices - chopped | Canned Chicken - Chopped | Cheese Ravioli |
| Jarred Baby Vegetable | Jarred Baby Vegetable | Jarred Baby Vegetable | |
| Applesauce | Bananas | Baby Fruit | |
| Bread/Crackers | Bread/Crackers | Bread/Crackers | |
| Parmalat | Parmalat | Parmalat | |
| 2 yrs. plus | Cheese Sandwich* | Canned Chicken Sandwich | Cheese Ravioli |
| Diced Fruit Cocktail | Diced Peaches | Diced Pears | |
| Graham Crackers | Graham Crackers | Graham Crackers | |
| Powered Milk | Powdered Milk | Powdered Milk |
Section 3. Emergency Department Surge Considerations and In–Patient Bed Assignments for Pediatrics during Disasters
Emergency Department Surge Considerations
and In–Patient Bed Assignments for
Pediatric Patients during a Disaster
Draft for Public Comment
Purpose:
These recommendations are intended to help hospitals prepare for surge capacity needs, such as additional bed resources and emergency department space allocation, which may arise in the event of a disaster involving Children. The section presents a model disaster scenario that can be scaled according to the predicted response of each individual hospital and includes general principles that should act as guidelines for all hospital disaster plans.
Section Contents:
- General Guidelines
- Transfer Considerations for Hospitals without Pediatric Intensive Care Units
- Recommendations for pre-planning interfacility transport
- Planning Scenario
- Emergency Department Surge Considerations and In–Patient Bed Assignments
- Emergency Department Surge capacity space requirements and pediatric in–patient bed assignment recommendations during a disaster are outlined for the following three types of hospitals
- Non-Trauma Hospitals with Pediatric Intensive Care Units
- Hospitals with General Pediatric Services but without a Pediatric Intensive Care Unit
- Hospitals without Pediatric Services
General Guidelines:
During a disaster the following steps should be undertaking to prepare for the reception and care of potential pediatric patients:
- Trigger hospital external disaster plan
- Identify and notify providers with pediatric clinical expertise
- MD, RN from Pediatrics, Family Medicine, Emergency Medicine, Surgery
- If no pediatric expertise – notify adult providers from all departments for a disaster
- Identify pediatric equipment, drug dosing guidelines, ventilators, availability of operating rooms, and pediatric ICU beds
- Prepare for stabilization and transfer of injured patients if more pediatric patients require admission than institution is able to handle
- If hospital is receiving or expects to receive more Children than institution can handle, immediately contact other hospitals with pediatric capability and capacity for possible transfer of patients
- Set up a family assistance area for family of victims and a separate area for media contact
- Know the hospital’s pediatric surge capacity i.e. when will institution run out of clinicians, equipment, medications, OR rooms, or ICU beds for the number and severity of expected pediatric patients
- Request transport teams, and more MD and RN staff to help as needed
- Upon Arrival of pediatric victims:
- Patients should be decontaminated prior to entering the hospital if chemical or radioactive contamination is suspected. If the hospital doesn’t have a decontamination shower, while still outside, remove all clothing and objects from the patient and wash with water, preferably warm, for several minutes. This can be done for all age groups. See Section 7. Decontamination of the Pediatric Patient for more detailed information concerning protocols for pediatric decontamination.
- It is recommended that all hospitals keep at least 5 cribs, port-a-cribs, or playpens in a storage area for use in possible pediatric disaster scenarios. However, many hospitals without a pediatric ward will be unlikely to have any cribs available. Use of adult beds may be considered if the following actions are taken:
- Children will have to be boarded in adult beds that have side rails.
- The bed should be set at the lowest possible height.
- The bed should be unplugged so the buttons to adjust the bed do not work.
- If pediatric patients are boarded on an adult ward, appropriate sized airway supplies (Ambu bags, face masks, endotracheal tubes, stylets, oral airways) chest tubes, Foley catheters, and over the needle IV catheters/IO needless should be available for each patient.
- Hospital administration and social work must plan for news media and a rush of anxious parents and family members.
- Security needs to be prepared to handle large numbers of family members and other non-medically affected individuals. Expect approximately four to five visitors/family per pediatric patient.
- Consider opening a Pediatric Safe Area to temporarily care for non-injured or discharged unaccompanied Children. See Section 1. Pediatric Security Issues during a Disaster.
- All attempts at identifying pediatric victims need to be made. See Child ID Survey Form located in Section 1. Security Considerations. A frequently updated list should be maintained and information relayed to the hospital emergency operating center and to the hospital family assistance center.
Transfer Considerations For Hospitals Without Pediatric Intensive Care Units
The transfer criteria for critical pediatric patients must be planned for in advance for hospitals that do not have Pediatric Intensive Care Units.
If a hospital does not have a Pediatric ED or a PICU, then any Child (especially young Child, infant or toddler) with a need for operative procedure or PICU care may require stabilization and transfer. These Children should to be identified by predetermined criteria. For example, this may include a trauma score (Pediatric Trauma Score or Revised Trauma Score), or need for other intensive level of care, such as: intubation, assisted ventilations, comatose, increased intracranial pressure, shock, inotropic support, ongoing seizures, or other major organ failure.
Prearranged agreements with ambulance agencies and receiving hospitals should be in place. Hospitals should have agreements with their traditional referral hospitals, but should also have agreements with those closest geographically or with the shortest transport routes since during a disaster transportation may be difficult due to traffic closure or other obstructions.
On–line Revised Trauma Score Calculator may be found at:
http://www.sfar.org/scores2/triss2.html ![]()
On–line Pediatric Trauma Score Calculator may be found at:
http://www.sfar.org/scores2/triss2.html ![]()
A sample of an interfacility transfer agreement can be found the California Emergency Medical Services Authority web site located at:
http://www.emsa.ca.gov/pubs/pdf/emsa186.pdf ![]() (PDF)
(PDF)
Planning Scenario
In order to prepare for the pediatric bed needs during a disaster, the CBPP Pediatric Task Force has created a disaster scenario to better describe the necessary bed resource demands that hospitals might expect.
Assume 40 pediatric patients of all ages arrive at Hospital A following an explosive disaster.
- 5 critically ill or injured (Red Tag)
- 10 moderately ill or injured (Yellow Tag)
- 25 minimally injured or uninjured (Green Tag)
The following sets of planning recommendations for emergency department surge capacity space and In–Patient bed assignments address three categories of hospitals:
- Non-Trauma Hospitals with a Pediatric Intensive Care Unit
- Hospitals with General Pediatric Units, but without Pediatric Intensive Care Units
- Hospitals without any Pediatric In–Patient Units
- Non-Trauma Hospitals with a Pediatric Intensive Care Unit
The following is a suggested plan for the distribution of pediatric victims upon arrival at a hospital with pediatric intensive care unit capability, but is not a certified trauma center. Hospitals must consider their own resources and personnel when creating their pediatric disaster plan.
Emergency Department Surge Considerations
Red tagged patients, or critical patients, should be placed in the most acute beds of their pediatric emergency area.
- When this area becomes saturated, remaining critical pediatric patients should go to the adult critical care areas in the emergency department
- In the absence of a trauma team, overall responsibility will be with the emergency department attendings with appropriate transfer to the PICU / pediatric ward attendings
- Pediatric surgery should be immediately consulted in the absence of a trauma team for patients with penetrating injuries to the abdomen or thorax. All other surgical specialties (neurosurgery, orthopedics, ENT, ophthalmology, etc.) should be placed on standby
Yellow tagged patients, those moderately injured or ill, should be placed in the non-acute care area of the pediatric emergency department with overflow going to non-acute care areas of the adult emergency department.
- Yellow tagged patients need to be treated and assigned disposition in a timely manner and reevaluated frequently to insure their condition does not deteriorate and warrant immediate medical intervention
Green tagged patients, minor or non-injured patients, should be triaged to the waiting room or to the pediatric clinic area or another large room capable of handling a large number, depending on day of week and time of disaster.
- Green tagged patients need to be re-evaluated frequently to insure their condition does not deteriorate and warrant immediate medical intervention
- When medically reasonable, green tagged patients should be discharged as soon as possible to an appropriately identified adult care giver as per hospital policy
Assignment of In–Patient Bed Space
The most critical cases and / or youngest victims should receive priority for Pediatric Intensive Care Unit beds. Once the PICU is full, overflow patients could be managed by Pediatrics in the Post Anesthesia Care Unit (PACU), if the patient required surgery, or in monitored beds on the pediatric ward or in adult medical or surgical ICUs.
Moderately injured or ill patients requiring admission should be admitted to the pediatrics ward until all beds are utilized. At that point, the hospital must decide to increase the ward census (add 1 more bed per room if space allows) or board the oldest pediatric patients on adult wards. If possible, all Children should board on the same adult ward for ease of nursing care and to improve the Children’s psychological well being.
- Hospitals with a General Pediatric Service but without a Pediatric Intensive Care Unit
The following is a suggested plan for the distribution of pediatric victims upon arrival at a hospital without pediatric intensive care unit (PICU) capability, but does have an In–Patient pediatric unit. Hospitals must consider their own resources and personnel when creating their pediatric disaster plan.
Most hospitals that do not have a PICU also do not have a dedicated pediatric emergency department. If your hospital has a pediatric emergency department, follow guidelines above. It is likely the hospital will have a general emergency department.
Emergency Department Surge Capacity Considerations
Red tagged patients, or critical patients, should be placed in the most acute care area of the emergency department.
- When that area becomes saturated, remaining critical patients should go to a monitored observation area in your emergency department.
- Overall responsibility will be with the emergency department attending and transferred to the pediatric ward attending.
- If the hospital has a trauma team, they should be immediately consulted and the trauma team attending will take responsibility for all Children requiring trauma surgery.
- Pediatric surgery should be immediately consulted in the absence of a trauma team for patients with penetrating injuries to the abdomen or thorax. All other surgical specialties (neurosurgery, orthopedics, ENT, ophthalmology, etc.) should be placed on standby.
Yellow tagged patients, moderately injured or ill, should be placed in the non- acute care areas of the emergency department with yellow tag overflow going to waiting room areas, or other designated ares, that are converted to patient care areas for the duration of the disaster.
- Yellow tagged patients need to be treated and assigned disposition in a timely manner and reevaluated frequently to insure their condition does not deteriorate and warrant immediate medical intervention.
- Admitted patients should be transferred up to the pediatric ward as soon as possible.
Green tagged patients, minimally on non-injured, should be triaged to the waiting room, lobby, or to the pediatric clinic area depending on the day of the week and time of disaster.
- Green tagged patients need to be reevaluated frequently to insure their condition does not deteriorate and warrant immediate medical intervention.
- When medically reasonable, green tagged patients should be discharged as soon as possible to an appropriately identified adult care giver as per hospital policy.
Assignment of In–Patient Bed Space for Hospitals without Pediatric Intensive Care Units
Pediatric critical care patients should be transferred to a hospital that can provide a higher level of care as soon as possible. Until transfer is completed, patients can be managed by Pediatric Staff in the post-operative recovery room, if the patient required surgery, or in monitored beds on the pediatric ward or in adult medical or surgical ICUs.
Moderately injured or ill Children requiring admission should be admitted to the pediatrics ward until all beds are utilized. At that point, the hospital must decide to increase the pediatric ward census (add 1 more bed per room if space allows) or board the oldest pediatric patients on adult wards. If possible, all Children should board on the same adult ward for ease of nursing care and to improve the Children’s psychological well being.
- Hospitals without a Pediatric Service
The following is a suggested plan for the distribution of pediatric victims upon arrival at a hospital without pediatric intensive care unit (PICU) capability or pediatric In–Patient wards. Hospitals must consider their own resources and personnel when creating their pediatric disaster plan.
It is recommended that all hospitals keep at least 5 cribs or playpens in a storage area for use in possible pediatric disaster scenarios. However, many hospitals without a pediatric ward will be unlikely to have any cribs available. Use of adult beds may be considered if the following actions are taken:
- Children will have to be boarded in adult beds that have side rails.
- The bed should be set at the lowest possible height.
- The bed should be unplugged so the buttons do not function.
All pediatric patients requiring admission should be transferred to a hospital that can provide a higher level of care as soon as it is medically and technically possible.
Unstable patients will require initial management at the receiving hospital where they first arrive prior to transfer.
Emergency Department Surge Capacity Considerations
Red tagged patients, or critical patients, should be placed in the most acute care area of the emergency department.
- When that area becomes saturated, remaining critical patients should go to a monitored observation area in your emergency department.
- Overall responsibility will be with the emergency department attending. If the hospital has a trauma team, they should be immediately consulted and the trauma team attending will take responsibility for all Children requiring trauma surgery.
- Adult surgery should be immediately consulted in the absence of a trauma team for patients with penetrating injuries to the abdomen or thorax as they will be the most capable service for immediate intervention. All other surgical specialties (neurosurgery, orthopedics, ENT, ophthalmology, etc.) should be called into the hospital or placed on standby.
Yellow tagged patients, moderately injured or ill, should be placed in the non-acute care areas of the emergency department.
- Yellow tagged patients need to be reevaluated frequently to insure their condition does not deteriorate and warrant immediate medical intervention.
- Yellow tag overflow should go to waiting room or other designated area that will be converted to patient care areas for the duration of the disaster.
- Patients requiring admission should be transferred up to adult In–Patient wards as soon as possible. The beds should be at the lowest possible height, have side rails, and have the electronic bed functions disabled so the buttons will not function.
Green tagged patients, minimally or non–injured,should be triaged to the waiting room, lobby, or to the adult clinic area depending on the day of the week and time of disaster.
- Green tagged patients need to be re-evaluated frequently to insure their condition does not deteriorate and warrant immediate medical intervention
- When medically reasonable, green tagged patients should be discharged as soon as possible to an appropriately identified adult care giver as per hospital policy.
Assignment of In–Patient Beds for a Hospital without a Pediatric Service
Pediatric critical care patients should be transferred to a hospital that can provide a higher level of care as soon as possible. Until transfer arrangements are completed, critical patients can be managed by Anesthesia in the recovery room, if the patient required surgery, or in adult medical or surgical ICU’s, or monitored beds on adult In–Patient wards until the patient can be safely transferred.
Non–critical patients requiring admission can be admitted to an adult ward if appropriate transfer is delayed or unavailable. If possible, all Children should board on the same adult ward for ease of nursing care and to improve the Children’s psychological well being.
Section 4. Equipment for Pediatric Disasters
Minimal Pediatric Equipment Recommendations for
Emergency Departments*
Draft for Public Comment
Purpose:
The following chart has been modified from the New York State 911 Hospital Receiving Guidelines1. The amounts given are the minimal recommended number of items per 1 expected critical patient in an emergency department. Each institution must determine what its expected surge capacity for pediatric critical patients is and should adjust inventory according to the number of patients for which it will plan. For example, if Hospital A decides to prepare for an influx of 4 critical pediatric patients, then the numbers in the amounts column should be multiplied by 4.
Additionally, many hospitals are creating and stocking disaster carts to be used in designated areas. It is recommended that hospitals also consider stocking a cart specifically for the emergency department for a Pediatric Critical Care Area.
*Amounts based on needs expected per 1 critical pediatric patient of unknown age or size
E = essential, D = desirable
| Minimal Pediatric Equipment Recommendations for Emergency Departments | ||
|---|---|---|
| Equipment Type | Amount | Importance |
| Ambu Bags | ||
| Infant | 2 | E |
| Child | 2 | E |
| Arm Boards | 2 | D |
| Blood Pressure Cuffs | ||
| Infant/Small Child | 1 | E |
| Chest Tubes | ||
| sizes 12F, 16F, 20F, 24F, 28F | 2 each size | E |
| Dosing Chart, Pediatric | 1 | E |
| ETCO2 Detectors (pediatric, disposable) | 2 | E |
| ET Tubes | ||
| 2.5 - 6.5 | 3 each size | E |
| Foley Catheters | ||
| sizes 8F, 10F, 12F | 2 each size | E |
| Gastrostomy tubes | ||
| sizes 12F, 14F, 16F | 2 each size | D |
| Infant Scale | 1 for any # patients | D |
| Intraosseous Needles | 3 | E |
| Intravenous Infusion Pumps | 1 | D |
| Laryngoscope Blades | ||
| Macintosh 0,1,2 | 2 each size | E |
| Miller 0,1,2 | 2 each size | E |
| Laryngoscope Handles (pediatric) | 2 | E |
| Face masks, clear self-inflating bag (500cc) | ||
| Infant | 2 | E |
| C hild | 2 | E |
| Non Rebreather | ||
| Infant | 2 | E |
| Child | 2 | E |
| Nasal cannula | ||
| Infant | 2 | E |
| Child | 2 | E |
| Nasogastric Tubes | ||
| sizes 6F, 8F, 10F, 12F, 14F, 16F | 2 each size | E |
| Nasopharyngeal Airways (all pediatric sizes) | 1 each size | D |
| Newborn Kit / Obstetric/Delivery Kit | 1 | E |
| Oral Airways (all pediatric sizes 00, 01) | 2each size | E |
| Over the Needle Intravenous Catheters | ||
| sizes 20, 22, 24 | 5 each size | E |
| Restraining Board (pediatric) | 1 | D |
| Resuscitation Tape, length based (Broselow) | 2 | E |
| Seldinger Technique Vascular Access Kit | ||
| sizes 4F, 5F, | 3 each size | D |
| Catheters 15cm length | 3 each size | D |
| Semi Rigid Cervical Spine Collars | ||
| Infant | 2 | E |
| Small Child | 2 | E |
| Child | 2 | E |
| Suction Catheters | ||
| 5F, 8F | 5 each size | E |
| Syringes, 60cc, catheter tip (for use with G/T tube) | 2 | E |
| Tracheostomy Tubes | ||
| sizes 00 to 6 | 2 each size | E |
| Warming Device (overhead warmer for newborns) | 1 | D |
- 1 Emergency Department Standards, Revised Sixth Edition, Fire Department, City of New York, Oct. 1997.
Section 5. Training for the Care of the Pediatric Population during a disaster
Training for Care of the Pediatric Population during a Disaster
Draft for Public Comment
Purpose:
The recommendations included in this section suggest training to ensure that pediatric patients receive appropriate care at all hospital facilities during a mass casualty, disaster, or terrorism related event. General medical and disaster training as well as pediatric–specific education options are included, all of which are recommended to enhance hospital response.
Section Contents:
- General Guidelines
- Training Recommendations
- Non-Trauma Hospitals with a PICU
- Hospitals with an In–Patient Pediatric Service but without a PICU
- Hospitals without an In–Patient Pediatric Service
- Training Recommendations Table
- List of Disaster and Emergency Training Courses
- Resource list of disaster and emergency training courses
General Guidelines:
Disaster and emergency training includes education in both the core principles of disaster management and the emergency treatment of adult and pediatric patients requiring basic, advanced, and trauma life support.
All hospitals should address the pediatric population when planning training courses for staff who will likely respond during a disaster. Additionally, the hospital disaster committee should consider the “pediatric surge capacity” of the current staffing, whether the hospital has pediatric services or not.
Training Recommendations
- Non-Trauma Hospitals with Pediatric Intensive Care Units
In the hospital disaster plan, these hospitals should plan for the ability to “surge” their pediatric inpatient capacity.
Pediatric In–Patient surge capacity might be accomplished through:
- Admission of additional patients to the existing pediatric unit(s)
- Utilization of non-clinical space for pediatric patient care
- Conversion of adult inpatient space (such as a surgical unit) to a temporary pediatric unit
Staffing anticipated to be assigned to these “pediatric inpatient surge capacity” areas, including but not limited to Pediatric ICU nurses and physicians, should have appropriate basic pediatric disaster training.
- Hospitals with Pediatric Service, but no Pediatric Intensive Care Unit
Hospitals with general pediatric In–Patient services should prepare for the same possibilities listed for hospitals with a PICU described above. In addition, critical pediatric patients might require intensive care and subsequent monitoring when transfer is not immediately possible.
Possible locations for temporary placement of critical pediatric patients include:
- Adult Medical Intensive Care Unit
- Adult Cardiac Care Unit
- Surgical Care Unit
- Post–Anesthesia Care Unit
- Other appropriate In–Patient intensive care unit
The staff anticipated to be responsible for the various levels of pediatric care should have the appropriate basic pediatric disaster training. Since pediatric intensivists and pediatric critical care nurses are not available at these facilities, the applicable training recommendations are recommended for Medical and Surgical ICU nurses and physicians.
- Hospitals without In–Patient Pediatric Services
These hospitals should develop disaster plans that address all of the possibilities for pediatric care listed above. While pediatric specialty staff may not be available normally at these facilities, it is recommended that certain staff be pre–identified and pre–designated to staff pediatric surge capacity areas. These predesignated individuals should receive appropriate training necessary to provide adequate care to the pediatric population during a disaster.
Training Recommendations
| Provider Level | Recommended Training: | ||||
|---|---|---|---|---|---|
| ACLS1 | ATLS2 | PALS3 | Basic Disaster Training4 | Disaster Drill including Pediatric Pts | |
| Emergency Department Nurses and Physicians | Yes | Yes | Yes | Yes | Yes |
| Pediatric Inpatient Unit Nurses and Physicians | Yes | No | Yes | Yes | Yes |
| Pediatric ICU Nurses and Physicians | Yes | No | Yes | Yes | Yes |
| Pediatric Surge Capacity Nurses and Physicians5 | Yes | No | Yes | Yes | Yes |
| Medical and Surgical ICU Nurses and Physicians6 | Yes | No | Yes | Yes | Yes |
| Other Surgical & Medical Physicians likely to respond to emergency department during disasters | Yes | Yes | Yes | Yes | Yes |
- Advanced Cardiac Life Support
- Advanced Trauma Life Support
- Pediatric Advanced Life Support
- “Basic Disaster Training” refers to an introductory or awareness level course covering the basics of individual risk assessment and response to Chemical, Biological, Radiological, Nuclear, and Explosive agents.
- “Pediatric Surge Capacity Nurses and Physicians” refers those staff designated as part of the hospital disaster plan to care for pediatric patients and their families in the event the usual hospital inpatient pediatric capacity is exceeded and these patients can not be transferred
- “Medical and Surgical ICU Nurses and Physicians” (or Recovery Room or other intensive care area) staff that might be required to care for critical pediatric patients who can not be transferred
Primary Disaster and Emergency Courses
American Heart Association Sponsored Courses:
http://www.americanheart.org/downloadable/heart/1125608700006ECC%20Course%20Matrix%202005.pdf ![]() (PDF)
(PDF)
Basic Life Support for Healthcare Providers (BLS)
- 1 day, all BLS providers, focuses on Cardiopulmonary Resuscitation (CPR) & Automatic External Defibrillator (AED)
Advanced Cardiac Life Support (ACLS)
- 2 days, all ACLS providers
Pediatric Basic Life Support (PBLS)
- 1 day, all PBLS providers, focuses on CPR/AED only
Pediatric Advanced Life Support (PALS)
- 2 days, all PALS providers
American College of Surgeons (ACS) Sponsored Courses): http://www.facs.org/trauma/atls/index.html ![]()
Advanced Trauma Life Support (ATLS)
- 2 days, physicians and physician extenders only
Disaster Courses
American Medical Association/National Disaster Life Support Foundation (AMA/NDLSF) Sponsored Courses:
http://www.ama-assn.org/ama/pub/physician-resources/public-health/center-public-health-preparedness-disaster-response/national-disaster-life-support/ndls-courses.shtml ![]() or http://www.bdls.com/
or http://www.bdls.com/ ![]()
Core Disaster Life Support (CDLS)
- 1/2 day, non medical hospital staff
Core Disaster Life Support-Decontamination (CDLS-D)
- 1 day, hospital decontamination team personnel
Basic Disaster Life Support (BDLS)
- 1 day, all medical disaster providers, soon to be available in an on-line version
Advanced Disaster Life Support (ADLS)
- 2 days, all medical disaster providers
Biological, Chemical, and Nuclear Emergencies Course (BCNE)
Sponsored by the Medical Society of the State of New York (MSSNY)
http://cme.mssny.org/rescenter.jsp ![]()
- 1/2 day seminar, also available in an extended on line version. Non-members are eligible to enroll
Hospital Emergency Response Training (HERT) for Mass Casualty Incidents (MCI) Train-the-Trainer Course
Sponsored by Department of Homeland Security at the Alabama Noble Training Center
http://training.fema.gov/EMIWeb/NTC/B960.asp ![]()
- Hospital Administrators, doctors, nurses, physicians, security personnel and other hospital staff who would make up or manage their Hospital’s Emergency Response Team, 2.5 to 3 day format
Additional Pediatric Emergency Courses
Advanced Pediatric Life Support (APLS)
Sponsored by the American Academy of Pediatrics/American College of Emergency Physicians (AAP/SCEP)
http://www.aplsonline.com/ ![]()
- 2 days, physicians, nurses, paramedics, covers basics of pediatric emergency medicine
Emergency Nursing Pediatric Course (ENPC)
Sponsored by the Emergency Nurses Association (ENA)
http://www.ena.org/coursesandeducation/CATNII-ENPC-TNCC/enpc/Pages/aboutcourse.aspx ![]()
- Modular course, self taught
Pediatric Education for Prehospital Professionals (PEPP)
Sponsored by the American Academy of Pediatrics (AAP)
http://www.peppsite.com/ ![]()
- 1 day, EMTs, 2 days, paramedics
Pediatric Terrorism Awareness Course
Sponsored by the University of Kentucky
http://www.kiprc.uky.edu/trap/peds.html ![]()
- Basic awareness course, available free and on-line, for EMS and emergency personnel
Prehospital Pediatric Care Course (PPCC)
Sponsored by the New York State Department of Health
http://www.health.ny.gov/nysdoh/ems/ppcctoc.htm ![]()
- 1 day, EMTs, 2 days, paramedics
Pediatric Prehospital Care Course (PPC)
Sponsored by the National Association of Emergency Medical Technicians (NAEMT)
http://www.naemt.org/education/epc_a.aspx ![]()
- 1 day, ATLS, 2 days, paramedics
Pediatric Disaster Life Support (PDLS)
Sponsored by the University of Massachusetts Medical School and Emergency Medical Services for Children (EMSC) Clearing House
http://www.umassmed.edu/index.aspx ![]()
- 1or 2-day training course for medical, EMS, and disaster professionals
Additional Trauma Courses
Trauma Nursing Core Course (TNCC)
Sponsored by the Emergency Nurses Association (ENA)
http://www.ena.org/coursesandeducation/CATNII-ENPC-TNCC/tncc/Pages/Default.aspx ![]()
- 2 days, nurses only
Advanced Trauma Care for Nurses (ATCN)
Sponsored by the Society of Trauma Nurses (STN)
http://www.traumanurses.org/education/atcn-courses.html ![]()
- 2 days, nurses only, run only in conjunction with a co-located ATLS course
Section 6. Transportation of Pediatrics during Disasters
Pediatric Population and Transport Issues during a Disaster
Draft for Public Comment
Purpose:
These recommendations suggest the appropriate procedure for the transportation of pediatric patients following a disaster. The section presents guidelines for both inter- and intra-hospital transport of stable and unstable pediatric victims. Pediatric patients may not always be accompanied by an adult during a disaster; therefore, these patients will require additional staffing and supply needs during their transport.
Section Contents:
- General Guidelines
- Transport of Pediatric Patients within the Hospital
- Transport Personnel
- Transport Equipment
- Chaperone and Safety Personnel
- Transport of Pediatric Patients from Hospital to Other Facilities
- Stable Patients
- Unstable Patients
- Table 6.1. Appropriate Use and Type of Car Seats
General Guidelines:
All hospitals need to plan for the potential necessity of delivering extended care to pediatric patients during a disaster. As part of this care, patients will need to be transported from clinical area to clinical area (including inpatient units) or to diagnostic testing (such as radiology, CT scan, and ultrasound). For those centers without specialized pediatric services, transfer of pediatric patients (after initial evaluation and stabilization) to a center with advanced pediatric capacity might be desired. However, transfer might not be possible due to local conditions and safety concerns, lack of appropriate transport vehicles and personnel, and/or lack of capacity at the usual pediatric resource hospitals.
Transport of Pediatric Patients within the Hospital
General guideline for transporting pediatric patients between hospitals units or diagnostic testing areas.
- Transport personnel:
- Personnel to transport stable patients
- All transport personnel should be oriented to special needs of pediatric transport
- Pediatric patients may not be left alone at any time
- Personnel to transport unstable patients
- Usual transport personnel
- Additional staff skilled in pediatric airway management and familiar with pediatric resuscitation
- Pediatric patients may not be left alone at any time
- Transport equipment:
- Airway management and resuscitation supplies available which are appropriate for all age groups (see Pediatric Equipment Recommendations)
- Identify appropriate transport vehicle:
- Adult stretchers may be appropriate for children >8-10 year old
- Smaller children may require crib, additional transport personnel, and/or converting an adult stretcher by adding padding to inside rails assure safety during transport
- Chaperone and safety personnel
- Parents or adult care givers should be encouraged to stay with children
- If no adult care giver is available, appropriate personnel must accompany and supervise pediatric patients to assure their safety at all times
- Patients on stretchers
- Patients less than 6 years old and not in appropriate crib require continuous 1:1 observation
- Patients 6 years and older should be evaluated for ability to follow safety rules while on stretcher
- Individual patients separated from other pediatric patients require constant 1:1 observation by staff
- Stable ambulatory patients
- May be co-horted in a Pediatric Safe Area with staff experienced or trained in observation of groups of children (such as school teachers, social workers, day care workers, etc.) See Section 1. Security for Pediatric Safe Area
- All ambulatory patients transported individually out of the Emergency Department require 1:1 adult supervision
Transport of Pediatric Patients from the Hospital to Other Facilities
During a disaster, the local conditions might preclude safe or efficient travel on the streets or highways or the usual pediatric receiving centers might be overwhelmed with patient volume and unable to accept transfers. Therefore, all hospitals must be prepared to provide emergent and continued pediatric care.
Even in the event that transfer to a pediatric center might be possible, the usual mechanisms for inter-hospital transfers should not be relied upon because these staff and equipment will be utilized to respond to the actual disaster. Therefore, hospitals should consider alternative mechanisms for safe pediatric transfers.
- Stable patients:
- Arrange for “Car Seats” including
- Rear facing for < 1 year old or < 20 pounds
- Forward facing for 1–4 years old and 20–40 pounds
- Booster seat for 4&ndash8 years old (or < 4’ 9” tall)
- Rear seat with seat belts for children 8–12 years old
- Children < 12 years old should not ride in the front seat
- Potential sources for appropriate car seats:
- Purchase or obtain through donation
- Identify local sources of car seats in case needed
- Survey employees to determine availability of car seats in employee vehicles
- Appropriate transport vehicles if ambulance not available:
- Cars, vans, city or private buses may be appropriate for children who can sit up (car seats may be necessary)
- School buses may be used for age 5 and over who can sit up
- Driver must be able to communicate with hospital emergency command center (cell phone or radio)
- Appropriate medical personnel (EMT, PA, NP, nurse, or physician) must accompany patients during transport
- Mental health personnel or staff trained in pediatric psycho-social needs should ideally accompany patients
- Unstable Patients or Potentially Unstable Patients
- Appropriate transport vehicle
- Emergency Medical Technician (EMT) or Paramedic ambulance augmented with:
- Hospital staff skilled in pediatric airway and resuscitation
- Equipment appropriate for age and acuity of patient (see Section 4. Equipment)
- Paramedic ambulance without additional hospital staff may be appropriate only for less critical patients
- Specialty pediatric transport teams from referral pediatric institutions
- Consider MOU with ambulance providers at distant locations (less likely to be involved with local disaster response)
Table 6.1. Appropriate Use and Type of Car Seats
| Infants | Toddler | Young Children | |
|---|---|---|---|
| Age & Weight | Up to 1 year old And 20 lb. or less. | Over 1 year to 4 years old And over 20 lb. | Ages 4–8, unless over 4' 9". And over 40 lb. |
| Seat Type | Infant only or rear-facing convertible | Convertible / Forward-facing | Belt positioning booster seat |
| Seat Positioning | Rear–facing only | Forward–facing | Forward–facing |
| Cautions: | All children age 12 and under should ride in the back seat. | ||
Section 7. Staffing Recommendations for Pediatrics in Disasters
Staffing Recommendations for Pediatrics during a Disaster
Draft for Public Comment
Purpose:
The recommendations included in this section address the critical issue of hospital staffing for pediatrics during a disaster. Appropriate allocation of personnel and the delegation of responsibilities are critical to mitigate the confusion and chaos created by disaster situations. Staffing considerations for pediatric patients during planning and permanent pediatric interest representation on the hospital Disaster Committee will greatly assist the facility to respond to the needs of pediatric patients. The following recommendations were created to primarily to address needs of institutions that do not have significant pediatric services or pediatric staff. When applicable, the HEICS positions should also be utilized by hospitals that have pediatrics.
Section Contents:
- General Guidelines
- Planning: Survey Staff for Pediatric Experiences
- Mitigation: Create Pediatric Leadership Positions
- Physician Coordinator for Pediatric Emergency Care in a Disaster
- Nursing Coordinator for Pediatric Emergency Care in a Disaster
- Response: Staffing for a Coordinated and Comprehensive Disaster Plan
- Sample HEICS Job Action Sheets
- Pediatric Services Unit Leader
- Pediatric Logistics Unit Leader
General Guidelines:
- Pre–identify hospital staff with specialty skills or experience in the treatment of pediatric patients.
- Develop a plan to utilize the specific skills of the above personnel, including call-down and notification procedures
- Create key pediatric positions these persons will occupy in a disaster event.
- Integrate the pediatric staffing plan into your hospital’s general Disaster /Emergency Response Plan.
Planning: Survey Staff for Pediatric Experiences
One of the first steps in appropriate pediatric planning is identifying members of your staff with pediatric skills and/or training. These members will become the primary pediatric caregivers. Ideally, these staff members with pediatric training and skills may come from pediatric emergency medicine, emergency medicine, pediatrics, or family medicine.
Other staff members with some pediatric experience in their specialty training and experience may be consider as an additional source of staffing. These staff members may include the following, but are not limited to, personnel trained in anesthesia, otolaryngology, pediatric surgery, trauma surgery, general surgery, orthopedics, urology, neurosurgery, and thoracic surgery.
Special attention must be paid to skills required for critical resuscitation procedures during the planning phase, especially for hospitals with limited pediatric specialty providers. Airway management, resuscitation, and critical care skills may be necessary during pediatric emergencies. Staff qualified to perform such procedures will be necessary during a disaster and should be identified in advance. For example, pediatric airway management may be performed by an anesthesiologist or otolaryngologist. Resuscitation and critical care medicine may be performed by anesthesiologists and general surgeons.
Included in this cadre of staff are nurses, physician assistants, and nursing assistants who work in the hospital’s emergency departments (EDs), operating rooms (ORs), post anesthesia care units (PACUs), intensive care units (ICUs), inpatient units, and outpatient clinics.
Staff members responsible for resuscitation in the EDs, ORs, PACUs, and ICUs should have the appropriate life support training certifications and corresponding hospital credentials. (See Section 6. Training.)
These pediatric response team members should be identified prior to a disaster and their names and contact information should be forwarded to the Disaster Committee and Command Center and maintained as a special call down sheet for pediatric disasters. Regular staff survey updates are needed to identify the staff member with this training and skill and to maintain current contact information.
Mitigation: Create Pediatric Leadership Positions for Key Personnel and Qualified Staff
These designated staff members will serve as the key personnel to coordinate the various elements of pediatric care and planning and serve as regular members of the Disaster Committee. Following are two key positions suggested for assignment to qualified clinical personnel:
- Physician Coordinator for Pediatric Emergency Care in a Disaster
- Nominated by the ED Medical Director and approved by the Disaster Preparedness Committee should be qualified to assume the following responsibilities:
- Ensure adequate skill and knowledge of staff physicians in emergency care and resuscitation of infants and children.
- Assist with development and periodic review of ED medications, equipment, supplies, policies, and procedures as member of general Disaster committee.
- Lead and assist with the development and updating of the hospital emergency response plan granting special attention to the needs of pediatric patients.
- Serve as liaison to appropriate in-hospital and out-of-hospital pediatric care committees in the community (if they exist).
- Serve as liaison to a definitive care hospital, which includes a regional pediatric referral hospital and trauma center, needed to integrate services or facilitate transfer for the continuum of care of the patient.
- Facilitate pediatric emergency education for ED health care providers.
- Identify in advance appropriately qualified staff who can accept responsibility for the immediate or extended care of pediatric patients during a disaster.
- During a disaster, will participate directly in emergency care and resuscitation of pediatric patients, in addition to the stated responsibilities.
- Nursing Coordinator for Pediatric Emergency Care in a Disaster
- Serve as liaison to appropriate in-hospital pediatric care committees.
- Serve as liaison to inpatient nursing as well as to a definitive care hospital, a regional pediatric referral hospital and pediatric capable trauma center for integrating services or to facilitate transfer for the continuum of care of the patient.
- Facilitate ED nursing continuing education in pediatrics and provide orientation for new staff members.
- Assist in development and periodic review of policies and procedures for pediatric care.
- Monitor pediatric equipment and medication availability.
- In a disaster, will participate actively in patient care through the emergency evaluation and management of children, in addition to stated responsibilities.
Response: Staffing for a Coordinated and Comprehensive Disaster Plan
Since many levels of staffing are required to respond adequately to a disaster involving pediatric patients, it is important that the designated team that will look after the welfare of the pediatric patients be as all-encompassing as possible. While the team will include such clinical staff as physicians, nurses and ancillary ED and in-patient personnel to provide emergency evaluation and treatment of children of all ages, additional staff may be called upon to respond to non-clinical pediatric patient needs in the hospital.
Included at the end of this chapter are Sample Job Action sheets that may be used to distribute tasks to staff designated to these ancillary leadership positions. Along with the Physician and Nursing Coordinators who will act as the point persons for clinical care in the ED , a general Pediatric Logistics Unit Leader and a Pediatric Services Unit Leader should also be assigned to monitor non-clinical areas. These Unit Leaders will facilitate accurate communication between non-clinical areas and oversee disaster response in areas such as Procurement, Materials/Supplies, Transportation, and Nutrition.
In planning to meet the immediate physical needs of the pediatric patient population during a disaster, hospitals may further prepare for child victims by considering psychological treatment that addresses their possible reactions to disaster including acute stress disorder, grief, and anger. With this in mind, it is recommended that hospitals prepare for the mental health needs of pediatric patients and coordinate a response plan that incorporates the skills of psychiatrists, psychiatric nurses, social workers and hospital chaplain. (See Section 10. Psychosocial Considerations for additional information).
Job Action Sheet
Pediatric Services Unit Leader
You report to:______________________________________(Operations Chief)
Command Center___________________________________________________
Mission:
To ensure that the pediatric treatment and holding areas are properly assigned, equipped, and staffed during an emergency
Immediate:
- Receive appointment from Unit Leader
- Read this entire job action sheet
- Obtain briefing from Unit Leader
- Gather external information from Treatment Area Supervisor/ED Charge Nurse regarding:
- Number of expected pediatric patients and their conditions
- Current total number of ED patients
- Expected time of patient arrival
- Determine number of available pediatric/crib beds [in-patine] and report to Operations Chief for planning purposes
- Determine 0n-site pediatric qualified staff members
- Determine additional staff needed based on expected patient volume
- Alert Discharge Unit Leader to institute early discharge/transfer of patients
- Initiate Pediatric Response Team as per plan:
- Predetermined Physicians for Pediatric Response (Pediatric/Family Practice/ Staff/ Community
- Predetermined Nurses (with pediatric experience and/or PALS/ENPC certification)
- Predetermined ancillary technicians with pediatric experience
- Others as predetermined
- Determine need for opening of a Pediatric Safe Area (dependent on expected number of unaccompanied children during the disaster)
- Assign Pediatric Safe Area Coordinator
- Communicate with Operations Chief to assure coordination of non–pediatric ancillary/support personnel as per the disaster plan
- Assure preparation of a pre–designated Pediatric Disaster Care Areas:
- Clear area
- Designate each specific area per plan and based on expected casualties
- Assure support personnel are assigned to each area
- Assure delivery of medical and non-medical pediatric equipment
- Assure set–up of pediatric equipment by clinical staff
- Receive pediatric patients
- Determine pediatric patient status
- Communicate findings to Treatment Area Supervisor for dissemination as per disaster plan
- Following triage of all children, move uninjured/unaffected children to pre–designated Pediatric Safe Area
Intermediate:
- Assess on-going staffing needs based on patient status report from:
- Pediatric healthcare personnel (emergency department, in-patient, and OR)
- non–pediatric ancillary /support personnel
- Pediatric Safe Area Coordinator
- Assess additional medical and non-medical equipment/supply needs
- Communicate with Pediatric Logistics Unit Leader via Operations Chief to Logistics Chief
- Assure delivery of needed supplies to pediatric designated areas
- Assess Pediatric Response Team basic needs:
- Food
- Rest
- Psychological support
- Obtain status of pediatric casualties (discharges, admissions, transfers, and Pediatric Safe Area) and report to Operations Chief
- Hold information sessions with Public Information Officer as needed
- Obtain Child Survey Forms (See Security Section) from all pediatric patients areas
- Report any unidentified or unaccompanied pediatric patients to Operations Chief
Extended:
- Debrief Pediatric Response Team and Pediatric Safe Area Coordinator regarding:
- Summary of Incident
- Review of areas of success
- Identify opportunities of success
- Thank and congratulate team
Job Action Sheet
Pediatric Logistics Unit Leader
You report to:________________________________________(Logistics Chief)
Command Center___________________________________________________
Mission:
To ensure that the pediatric needs are addressed by Procurement, Transportation, Materials Supply, and Nutritional Supply during an emergency
Immediate:
- Receive appointment from Logistics Chief
- Read this entire job action sheet
- Obtain briefing from Logistics Chief
- Number of expected pediatric patients and their conditions
- Timeline for supply needs
- Depending on the extent of HEICS activation, meet with Logistics Chief and distribute tasks to the following Unit Leaders:
- Procurement Unit Leader:
- Receive briefing from Logistics Chief and Pediatric Logistics Unit Leader
- Initiate Procurement Disaster Call list if warranted
- Work with vendors for pediatric supplies including hospital vendors and community resources (local pharmacies and grocery stores) for back–up resources
- Transportation Unit Leader:
- Receive briefing from Logistics Chief and Pediatric Logistics Unit Leader
- Initiate Transportation Disaster Call list if warranted
- Count open stretchers, carts, cribs, and wheelchairs for pediatric transportation
- If adult transport equipment options are used, ensure all are appropriately modified and safe for pediatric transport
- Report transportation options to Logistics Chief
- Coordinate delivery of transportation options to designated pediatric area or ED depending on scenario
- Designate transporters as needed from CS staff or Labor pool
- Ensure that all transporters are aware of pediatric safety issues and are not to leave pediatric patients unattended (see Section 6. Transport for more information)
- Materials/Supplies Unit Leader:
- Receive briefing from Logistics Chief and Pediatric Logistics Unit Leader
- Initiate Materials/Supplies Disaster Call list if warranted
- Collect and coordinate essential pediatric medical equipment and supplies
- Assist in preparation of pre–designated Pediatric Disaster Care Areas with Pediatric Services Unit Leader (See Section 4. Equipment Recommendations for more information)
- Assist in preparation of pre–designated Pediatric Safe Area with Pediatric Services Unit Leader (See Section 1. Security Issues for more information)
- Nutritional Supply Unit Leader: (See Section 2. Dietary for additional
- Receive briefing from Logistics Chief and Pediatric Logistics Unit Leader
- Initiate Nutritional Call list if warranted
- Estimate number of pediatric meals needed for 48 hours (See Section 2. Dietary for more information)
- Estimate pediatric food/snacks/hydration needs for Pediatric Safe Area
Intermediate:
- Obtain regular updates from Logistics Chief
- Assess additional equipment/supply needs for pediatrics
- Address pediatric concerns, questions and issues as needed
Extended:
- Document actions and decisions, submit reports to Logistics Chief
- Participate in debriefing
- Review areas of success
- Identify opportunities for improvement
- Thank and congratulate team
Section 8. Decontamination of the Pediatric Patient
Decontamination of the Pediatric Patient
Draft for Public Comment
Purpose:
These recommendations are intended to assist planning for the needs of all children presenting to any hospital (during a disaster or terrorist attack requiring decontamination) to be properly decontaminated in a timely manner. Children require special considerations that may not be addressed in the general Hospital Decontamination Plan.
Section Contents:
- General Guidelines
- General decontamination considerations recommended for all children
- Decontamination Recommendations Based on Age of Child
- Recommended procedures for decontamination of ambulatory and non-ambulatory children based on estimated age
- Children less than 2
- Children 2 to 8 years of age
- Children 8 to 18 years of age
- Model Decontamination Algorithm
- Graphical representation of pediatric decontamination procedures
- References
General Guidelines:
Infants and children have unique needs that require special considerations during the process of hospital-based decontamination.
- Separation of families during decontamination should be avoided, especially under conditions of large number of patients in a chaotic situation but medical issues take priority.
- Older children may resist or be difficult to handle out of fear, peer pressure, and modesty issues (even in front of their parents or caregivers).
- If the water temperature is below 98°F, the risk of inducing hypothermia increases proportionately with the smaller, younger child.
- Attention to airway management is a priority throughout decontamination showers.
- It cannot be assumed that the parents or caregivers will be able to decontaminate both themselves and their children at the same time (“hot zone” personnel should recognize the need to assist them).
- Large volume, low pressure water delivery systems (e.g. handheld hose sprayers) that are “child friendly” should be incorporated into the hospital decontamination showers.
- The smaller the child, the bigger the problemregarding any of these considerations such as hypothermia, airway management, separation of families, and ability to effectively decontaminate the child.
Decontamination Recommendations Based on Age of Child:
- Children are divided into three groups by ages: 8–18 years old (school age), 2–8 years old (pre–school), and 0–2 years old (infants and toddlers).
- The following recommendations are based on the estimated child’s age, since asking may be impractical due to the limitations of the PPE worn by decontamination team members or to a large influx of patients.
- The following recommendations are meant as general guidelines.
- Children less than 2 years of age (infants and toddlers):
Infants and toddlers represent the most challenging group in which these special needs considerations are the most important.
- All infants and toddlers should be placed on a stretcher and disrobed by either the child’s caregiver or “hot zone” personnel. All clothes and items that cannot be decontaminated should be placed in appropriate containers or bags as provided by the hospital and labeled.
- Each child should then be accompanied through the decontamination shower by either the child’s caregiver or “hot zone” personnel to ensure the entire patient is properly decontaminated. It is not recommended that the child be separated from family members or adult caregiver. It is not recommended that the caregiver carry the child due to the possibility of injury resulting from a fall, or from dropping a slippery and squirming child.Special attention must be given to the child’s airway while in the shower.
- Non-ambulatory children will be placed on a stretcher by “hot zone” personnel and disrobed (using trauma shears if necessary). All clothes and items that cannot be decontaminated should be placed in appropriate containers or bags as provided by the hospital and labeled.
- Each non-ambulatory child should then be escorted through the decontamination shower by either the child’s caregiver or “hot zone” personnel to ensure the entire patient is properly decontaminated. Special attention must be paid to the child’s airway while in the shower.
- Once through the shower, the child’s caregiver or “cold zone” personnel will be given a towel and sheets to dry off the child, and a hospital gown. Immediately, the child should be given a unique identification number on a wristband and then triaged to an appropriate area for medical evaluation.
- Children and their families (parents or caregivers) should not be separated unless critical medical issues take priority.
- Children 2 to 8 years of age (pre-school):
From age 2 to 8, children should be able to walk and speak, yet will still look like a child with considerable variations in physiology and anatomy.
- Ambulatory children should be assisted in disrobing by either the child’s caregiver or “hot zone” personnel. All clothes and items that cannot be decontaminated should be placed in appropriate containers or bags as provided by the hospital and labeled.
- Each child should be directly accompanied through the shower by either the child’s caregiver or “hot zone” personnel to ensure the entire patient is properly decontaminated. It is recommended that the child not be separated from family member(s) or the adult caregiver.
- Non-ambulatory children should be placed on a stretcher by “hot zone” personnel and disrobed (using trauma shears if necessary). All clothes and items that cannot be decontaminated should be placed in appropriate containers or bags as provided by the hospital and labeled.
- Each non-ambulatory child on a stretcher is escorted through the decontamination shower and assisted with decontamination to ensure the entire patient is properly decontaminated.
- Once through the shower, each child should be given a towel and sheets to dry, and a hospital gown. Immediately, the child should be given a unique identification number on a wristband and then triaged to an appropriate area for medical evaluation.
- Children and their families (parents or caregivers) should not be separated unless critical medical issues take priority.
- Children 8 to 18 years of age (school age):
At the age of 8 years and upward, the airway anatomy approximates that of an adult. Although it is tempting to regard this age group as “small adults” – there are special needs unique to this age group.
- Ambulatory children should disrobe when instructed to do so by “hot zone” personnel. All clothes and items that cannot be decontaminated should be placed in appropriate containers or bags as provided by the hospital and labeled.
- Each child should then walk through the decontamination shower, preferably in succession with their parent or caregiver, and essentially decontaminate him/herself.
- Non-ambulatory children should be placed on a stretcher by “hot zone” personnel and disrobed (using trauma shears if necessary). All clothes and items that cannot be decontaminated should be placed in appropriate containers or bags as provided by the hospital and labeled.
- Then each non-ambulatory child is escorted through the decontamination shower and assisted with decontamination to ensure the entire patient is properly decontaminated.
- Once through the shower, each child will be given a towel and sheets to dry, and a hospital gown. Immediately, the child should be given a unique identification number on a wristband and then triaged to an appropriate area for medical evaluation.
- Children and their families (parents or caregivers) should not be separated unless critical medical issues take priority.
Hospital Decontamination and the Pediatric Patient
Model Protocol Algorithm
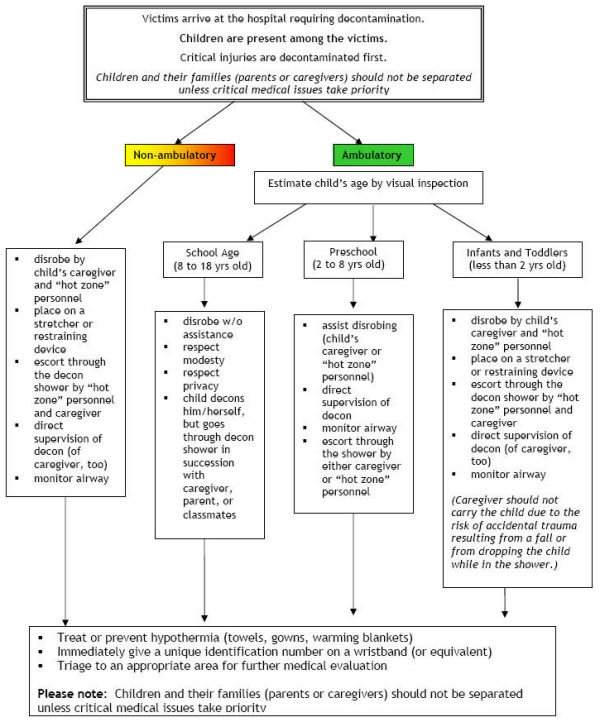
References
- Occupational Safety and Health Administration (OSHA), 29 CFR 1910.120, Hazardous Materials Incident Response Curriculum Guidelines (HAZWOPER), last updated Directive 11/05/2003. http://www.osha.gov/

- OSHA Best Practices for Hospital-based First Receivers of Victims from Mass Casualty Incidents Involving the Release of Hazardous Substances, December 2004. http://www.osha.gov/dts/osta/bestpractices/firstreceivers_hospital.html

- U.S. Department of Health and Human Services: Concept of Operations Plan (CONOPS) for Public Health and Medical Emergencies, March 2004, Tommy G. Thompson, Secretary Dept. HHS. http://www.hhs.gov/disasters/discussion/planners/conops.html

- Okumura T, Takasu N, Ishimatsu S, Miyanoki S, Mitsuhashi A, Kumada K, Tanaka K, Hinohara S. Report on 640 victims of the Tokyo subway sarin attack. Ann Emerg Med 1996 Aug;28(2):129-35
- MacIntyre AG, Christopher GW, Eitsen E, Gum R, Weir S, DeAtley C, Tonat K, Barbera JA. Weapons of mass destruction events with contaminated casualties. JAMA 2000; 283:242-249.
- Barbera JA, MacIntyre AG. Mass Casualty Handbook: Hospital, Emergency Preparedness and Response, First edition 2003: Jane’s Information Group, Ltd.
- Hick JL, Hanfling D, Burnstein J, Markham A, McIntyre G, and Barbera JA. Protective equipment for health care facility decontamination personnel: regulations, risks, and recommendations. Ann Emerg Med Sept 2003; 42(3):370-380
- Hick JL, Penn P, Hanfling D, Lapp MA, O’Laughlin D, Burnstein JL. Establishing and training health care facility decontamination teams. Ann Emerg Med 2003 Sept; 42(3):381-390
- Markenson D. Redlener I. Pediatric Preparedness for Disasters and Terrorism: A National Consensus Conference. Executive Summary 2003. National Center for Disaster Preparedness. Columbia University, Mailman School of Public Health http://www.bt.cdc.gov/children/pdf/working/execsumm03.pdf
 (PDF)
(PDF) - Testimony before the Senate Committee on Health, Education, Labor, and Pensions Subcommittee on Children and Families Presented by Joseph L. Wright, MD, MPH, FAAP on Behalf of the American Academy of Pediatrics. Senate Committee on Health, Education, Labor, and Pensions Subcommittee on Children and Families. Washington, DC: American Academy of Pediatrics, 2001 of the United States Senate http://www.aap.org/terrorism/resources/academy_resources.html
Section 9. Pharmacy Needs of Pediatrics in Disasters
Pharmacy Needs for Pediatrics in Disasters
Draft for Public Comment
Purpose:
The recommendations included in this section focus on pediatric pharmacy inventory and drugs which are likely to be used during a pediatric emergency. The list of medications and the daily pediatric dosages for relevant indications are provided to help pharmacists planning an inventory, but they cannot replace comprehensive treatment and prophylaxis guidelines. The following content is based on reference material from the CDC, AAP, FDA, the National Center for Disaster Preparedness, and the CDER at the NIH. It is recommended that hospitals consult with the CDC and regional health departments for the most up-to-date treatment guidelines. A reference section has also been included with links to clinical pathways for some important biological exposures.
Section Contents:
- General Guidelines
- General recommendations for hospitals for maintenance of pharmaceutical inventory
- Pharmacy Inventory (Pediatrics)
- Lists of medication and daily pediatric doses relevant for disaster planning
- Drug Preparation and Dosing
- Useful tables for the pediatric preparation and dosing of the following drugs:
- Table 8.1 Doxycycline suspension
- Table 8.2 Sodium nitrate
- Table 8.3 Oseltamvir
- Table 8.4 Potassium Iodide Solution
- Table 8.5 ThyroShield Dosing Recommendations
- Table 8.6 Mark-1 Kit Use in Pediatrics – NYC Protocol
- References and Web Sites
General Guidelines:
The following are recommendations and guidelines for the maintenance of pediatric inventories for pharmaceuticals most likely to be needed during disasters:
- Establish procedures for maintenance of pharmacy disaster carts (kits/bags) for pediatric patients.
- Maintain inventory of essential pharmaceuticals (72-hour supply).
- Estimate supply for treatment or exposure prophylaxis of biologic agents at the facility:
Number of courses of treatment = (Daily census of pediatric patients) +
(Potential pediatric disaster victims) +
(Consider pediatric family members of hospital staff)
- Provide appropriate facility for storage of inventory.
- Inspect bags/cart monthly for integrity, quantities of drugs, record date of inspection on a maintenance record.
- Plan for re-supply from local and state stockpiles; collaborate with regional emergency management planners.
- Evaluate existing MOUs, network affiliations, local pharmacies, drug companies; maintain a list on the cart of these sources of additional drugs.
- As per HEICS, identify unit leader/director responsible for distribution of medications in case of disaster.
- Develop criteria to stop nonessential use of antibiotics until stockpile arrives and is distributed.
- Regularly test pharmacy during drills.
Pharmacy Inventory (Pediatrics)
Abbreviations: E = essential, D = desired, mg = milligram, g = gram, kg = kilogram, ml = milliliter, BID = twice daily, q = every, h = hours, div = divided (for dosages based on a daily dose, which needs to be then divided into intervals), max = maximum dose, y/o = years old, IV = intravenous, IM = intramuscular, PO = by mouth, SC = subcutaneous, IO = intraosseous (note: as an alternative to the IV route in patients with vascular access problems most parenteral medications can be given via an intraosseous needle), PRN = as needed.
Many of these medications may already be in hospital’s pharmaceutical inventory.
| Exposure/Agent | Pediatric Dose | Importance |
|---|---|---|
Anthrax, pulmonary Ciprofloxacin3 Anthrax, cutaneous Anthrax, post-exposure Prophylaxis |
10-15 mg/kg IV q12h (max 1g/day) 2.2 mg/kg IV q12h (max 100mg/day) 10-15 mg/kg IV q12h 250,000 – 600,000 units/kg/day div q4h 10-15 mg/kg IV q12h (max 1g/day) 2.2 mg/kg IV q12h (max 100mg/day) 25-50 mg/kg/day PO div q6h 40-80 mg/kg/day PO div q8h 10-15 mg/kg PO q12h (max 1g/day) 2.2 mg/kg PO q12h (max 200mg/day) |
E E E E E E D D E E |
Brucellosis, serious infections Streptomycin or |
15 mg/kg IM q12h (max 2g/day) 20 mg/kg/day PO/IV div q12/24h 2.5 mg/kg IV/IM every 8 hr (term neonates 1 week of age, infants/children <5 y/o) 2-2.5 mg/kg IV/IM every 8 hr 15 mg/kg IV q12h |
D E E E |
Brucellosis, less serious infections Trimethoprim-Sulfamethoxazole |
5 mg/kg TMP component q12h PO |
E |
Influenza, prophylaxis 9 Oseltamivir 12mg/ml oral suspension |
75 mg PO daily 4.4 to 8.8 mg/kg/day PO daily |
D D |
Influenza, therapy 9 Oseltamivir 12mg/ml oral suspension |
See Table 3 for dosing Same as prophylaxis (max 200mg/day) |
D D |
Iodine Radionuclide Exposure Potassium iodide (KI) |
See Table 4 for preparation 4 See Table 5 for dosing 8 |
E D |
Nerve Agents Pralidoxime 1g/20ml Atropine sulfate Inj. 1 mg/10 ml Atropine/Pralidoxime Autoinjector (Mark-I) 6 |
25-50mg/kg IV/IM (max 1g IV, 2g IM), repeat within 30-60min, then q1h x 1-2 doses PRN 0.05-0.1mg/kg IV/IM (min 0.1mg, max 5mg) see table 6 for dosing |
E E D |
Plague Gentamicin |
2.5 mg/kg IV q8h 15 mg/kg IM q12h 2.2 mg/kg IV q12h (max 200mg/day) 5 mg/kg IV q12h |
E D D D |
Plague meningitis Chloramphenicol |
25 mg/kg IV q 6h (max 4g/day) 11 |
D |
Plague, post-exposure prophylaxis Doxycycline 2 |
2.2 mg/kg PO q12h (max 100mg) 20 mg/kg PO q12h (max. 1g/day) |
E E |
Pneumonia Plague Doxycycline 2 |
2.2 mg/kg PO q12h (max 200mg/day) 20mg/kg PO q12h |
E E |
Pneumonic Tularemia Gentamicin 10 |
2.5 mg/kg IV q8h 15 mg/kg IM q12h 2.2 mg/kg IV q12h (max 200mg/day) 15 mg/kg IV q12h (max 1g) 15 mg/kg IV q6h (max 4g) 11 |
E D D D D |
Pulmonary Agents Sodium bicarbonate 4.2% and 7.5% Sodium nitrate 3% 5 Sodium thiosulfate 25% |
1mEq/kg/dose (2ml/kg of 4.2% sol. (for neonates) or 1.1ml/gk of 7.5% sol.) IV/IO See table 2 for dosing 1.65 ml/kg (max 50ml) |
E E E |
Viral Hemorrhagic Fever |
Ribavirin 1 |
D |
| Analgesics | Pediatric Dose | Importance |
Acetaminophen 80,160mg/0.8ml oral solution Ibuprofen 100mg/5ml oral solution Morphine Inj. 1mg/ml Morphine 10mg/ml oral solution |
10-15 mg/kg q4h 5-10 mg/kg q6h 0.1-0.2 mg/kg IM/IV/SC q2-4h 0.2-0.5mg/kg q4-6h PRN |
E E E E |
| Emergency Drugs | Pediatric Dose | Importance |
Albuterol 2.5mg/3ml nebulizer solution Artificial Tears Eye Drops Atropine sulfate Inj. 1mg/10 ml Bacitracin ointment Calcium Chloride 10% Inj. 1g/10ml Dexamethasone Inj. 4mg/ml Dextrose 50% Inj. 25g/50ml Diazepam Inj. 10mg/2 ml Diphenhydramine Inj. 50mg/ml Dopamine Inj. 200mg/5ml Epinephrine (1/10,000) Inj. 0.1 mg/ml for cardiac arrest Furosemide Inj. 10mg/10ml Ketamine Inj. 10mg/ml Lidocaine 2% Inj., 5ml Mannitol 25% Inj. 12.5g, 50ml Midazolam Inj. 1mg/ml Phenytoin Inj. 250mg/5ml Prednisone 5mg/5ml syrup Silver Sulfadiazine cream |
<1y: 0.05-0.15 mg/kg q4h PRN Topical symptomatic care 0.02 mg/kg IV/IO/IM (min 0.1mg, max 0.5mg (child), max 1mg (adolescent) Topical wound/burn care 20 mg/kg (0.2ml/kg) slow IV/IO 0.5-2mg/kg/day IV/IM div q6h 0.25-1g/kg (0.5-2ml/kg) IV/IO 0.05-0.3mg/kg (max 10mg) IV 1.25mg/kg IV q6h 2-20 microgram/kg/minute IV 0.01mg/kg IV/IO 0.5-2mg/kg IV 2-3mg/kg IM loading dose: 1mg/kg IV/IO 0.25g/kg/dose IV over 30 minutes 0.1-0.2mg/kg (max 10mg) IV/IM 15-20mg/kg IV loading dose 2mg/kg/day PO div BID topical burn care |
E D E D E E E E E E E E E E E E E E E |
Footnotes
- Ribavirin IV: loading dose 30 mg/kg IV once (max. dose 2g), then 16 mg/kg IV (max. dose 500 mg) q6h for 4 days, then 8 mg/kg (max. dose 500 mg) for 6 days; Ribavirin PO: loading dose of 30 mg/kg PO once, then 15 mg/kg/day PO div q12 for 10 days
- See Table 1 for doxycycline suspension recipe
- Ciprofloxacin is the preferred agent, safety and effectiveness for this indication have been established in children (Meyerhoff et al, 2004); it is also recommended for use in pregnant women; amoxicillin may be considered as an alternative in children (MMWR 2001)
- See Table 4 for KI suspension preparation and dosing
- See Table 2 for sodium nitrate dosing
- See Table 6 for Autoinjector usage
- See Table 5 for dosing of TyroShieldTM
- See Table 3 Oseltamvir Dosing for details
- Streptomycin or gentamicin is the preferred choices
- Serum concentrations should be maintained between 5-20 microgram/ml; concentrations over 25 microgram/ml can cause reversible bone marrow suppression
Drug Preparation and Dosing
Table 8.1: Doxycycline suspension preparation (adapted from FDA reference material, 2005): The second column indicates the portion of a tablet, which needs to be crushed and suspended for an individual patient in order to achieve the desired milligram concentration indicated in column 1. Columns 3 and 4: Dosage uniformity determination: analysis of crushed tablets mixed with low fat chocolate milk.
| Dosage (Mg) | Tablet Portion | Mg Doxycycline: Average and SD | Mg Doxycycline: Range |
|---|---|---|---|
| 100 Mg | 1 | 96.1+/-0.6 | 95.6-96.7 |
| 75 Mg | ¾ | 67.8+/-3.1 | 64.4-70.5 |
| 50 Mg | ½ | 47.0+/-2.4 | 42.9-49.5 |
| 25 Mg | ¼ | 23.8+/-3.5 | 18.3-32.1 |
* % Desired Dosage based on an average tablet assay of 97% equating to 100% dosage.
Table 8.2: Sodium nitrate dosing (Berlin et al, 1970)
| Estimated Hgb (g/dl) for average child | Sodium nitrate (3%) Dosage (ml/kg) |
|---|---|
| 7 | 0.19 |
| 8 | 0.22 |
| 9 | 0.25 |
| 10 | 0.27 |
| 11 | 0.30 |
| 12 | 0.33 |
| 13 | 0.36 |
| 14 | 0.39 |
| Maximum 10 ml |
Oseltamivir Dosing Recommendations For Children
Oseltamivir is not approved in children < 13 years for prophylaxis of influenza, but is approved for treatment in children over 1 year of age. Amantadine is cheaper than oseltamivir and approved in children > 1 year, but is only active against Influenza A. See Table 3 for the dosing of oseltamivir for therapy of influenza.
Table 8.3: Influenza treatment with oseltamivir (CDC, 2002; Prod Info Tamiflu(R), 2001)
| Weight* | Dose |
|---|---|
| >1 year, ≤ 15 kg | 30 mg BID |
| > 15 kg to 23 kg | 45 mg BID |
| > 23 kg to 40 kg | 60 mg BID |
| > 40 kg | 75 mg BID |
Solution Preparation For 65 Mg Potassium Iodide Tablet
(FDA reference material)
Preparation of mixture using 65mg KI tablets:
- Grind the potassium iodide 65 mg tablet into powder
- Put one 65mg potassium iodide tablet into a small bowl and grind it into a fine powder using the back of the metal teaspoon against the inside of the bowl. The powder should not have any large pieces.
- Mix potassium iodide powder into a Drink
- Add four teaspoonfuls of water to the potassium iodide powder in the small bowl. Use a spoon to mix them together until the potassium iodidepowder is dissolved in the water.
- Mix drink of choice with potassium iodide powder and water solution
- Add four teaspoonfuls of drink to the potassium iodide powder and water mixture described in Step 2.
The amount of potassium iodide in the drink is 8.125 mg per teaspoon. The number of teaspoonfuls of the drink to give your child depends on your child's age. Table 3 shows how many teaspoonfuls of potassium iodide mixture to give to an adolescent, child, or infant.
Please pay attention to the number of teaspoonfuls recommended when using a potassium iodide 65 mg tablet as it is different from the number of teaspoonfuls given when using a potassium iodide 130 mg tablet.
Table 8.4: Recommended doses of KI for children and infants with predicted thyroid radioactivity exposures equal to or greater than 5 cGy1, using 65 mg tablet preparations.
| If your child is: | Give your child this amount of potassium iodide (KI) * | Which is |
|---|---|---|
| Between 4 and 12 years old | 8 teaspoonfuls (Not tablespoonfuls) | 65 mg of potassium iodide (KI) |
| Over 1 month through 3 years | 4 teaspoonfuls (Not tablespoonfuls) | 32.5 mg of potassium iodide (KI) |
| An infant from birth through 1 month | 2 teaspoonfuls (Not tablespoonfuls) | 16.25 mg of potassium iodide (KI) |
* The amount to give your child for one dose. You should give your child one dose each day.
1 FDA, Guidance: Potassium Iodide as a Thyroid Blocking Agent in Radiation Emergencies, December 2001.
Thyroshieldtm Dosing Recommendations For Children
Table 8.5: Manufacturer’s dosing recommendation for ThyroShieldTM (table from Consumer Package Insert); available from Fleming & Company, Pharmaceuticals, Fenton, St. Louis Co., MO 63026, 1-800-343-0164
| Dose: |  |
|
| Adults over 18 years | 2 mL every day (130 mg) | |
| Children over 12 years to 18 years who weigh at least 150 pounds | 2 mL every day (130 mg) | |
| Children over 12 years to 18 years who weigh at less than 150 pounds | 1 mL every day (65 mg) |  |
| Children over 3 years to 12 years | 1 mL every day (65 mg) | |
| Children over 1 month to 3 years | 0.5 mL every day (32.5 mg) |  |
| Babies at birth to 1 month | 0.25 mL every day (16.25 mg) |  |
Take KI every day (every 24 hours) as directed by public officals. Don not take more than 1 dose in 24 hours. More will not help you. Too m uch medicaine may increase the chances of side effects.
Mark-1 Kit Use In Pediatrics
New York City Protocol for Infants and Children in a Nerve Gas Release
Most published recommendations for treatment of pediatric nerve agent poisoning are based upon standard resuscitation doses for these agents. However, certain medical and operational concerns suggest that an alternative approach may be warranted for treatment of children by emergency medical personnel following mass chemical events. 1) There is evidence both that suprapharmacologic doses may be warranted and that side effects from antidote overdosage can be tolerated. 2) There is concern that many emergency medical personnel will have difficulty determining both the age of the child and the severity of the symptoms. Therefore, the Regional Emergency Medical Advisory Committee (REMAC) of New York City and the Fire Department, City of New York (FDNY), Bureau of Emergency Medical Services, in collaboration with the Center for Pediatric Emergency Medicine (CPEM) of the New York University School of Medicine and the Bellevue Hospital Center, have developed a pediatric nerve agent antidote dosing schedule that addresses these considerations. This schedule is reproduced in the Table that follows:
Table 8.6: NYC Protocol for Infants and Children in a Nerve Gas Release
| Tag Color | Exposure, Respiratory Distress, Agitation, SLUDGEM | Atropine and 2-PAM Doses Monitoring Interval | Atropine Repeat Dosing | |
|---|---|---|---|---|
| RED (Pediatric) | Yes | Age <1 years |
1 Peds Atropine Auto-injector(0.5 mg) No 2-PAM Monitor every 3 minutes |
Atropine every 3 minutes as needed |
| Age 1-8 years |
1 Atropine Auto-injector (2mg) 1 2-PAM Auto-injector (600 mg) Monitor every 3 minutes |
|||
GREEN (Pediatric) |
No | None Monitor every 10 minutes for evidence of exposure | ||
| Note: Treatments Listed Above are for Patients < 8 Years Old Only | ||||
These doses are comparable to those being administered to adults with severe symptoms and within limits deemed tolerable following accidental nerve agent overdose in children. We conclude that the above approach is likely a safe and effective alternative to weight based dosing of children, which will be nearly impossible to attain under field conditions.1.
1. Foltin G et al. Pediatric Nerve Agent Poisoning: Medical and Operational Considerations for Emergency Medical Services in a Large American City, Submitted for publication May 2005.
References and Web Sites
References:
Berlin CM. The treatment of cyanide poisoning in children. Pediatrics 1970;46:793-6.
Goldfrank LR et al (eds.). Goldfrank’s Toxicologic Emergencies (7th edition). McGraw-Hill 2002.
Markenson D and Redlener I. Pediatric Terrorism Preparedness National Guidelines and Recommendations: Findings of an evidence-based consensus process. Biosecurity and bioterrorism strategy, practice, and science 2004;2(4):301-319.
Meyerhoff A, Albrecht R, Meyer JM, Dionne P, Higgins K, Murphy D. US Food and Drug Administration approval of ciprofloxacin hydrochloride for management of postexposure inhalational anthrax. Clin Infect Dis 2004;39:303-8.
MMWR Morb Mortal Wkly Rep. 2001;50(45):1014-6.
National Emergency Medical Services for Children Resource Alliance, Committee on Pediatric Equipment and Supplies for Emergency. Guidelines for pediatric equipment and supplies for emergency departments. Ann Emerg Med. 1998;31:54-57.
Patt HA and Feigin RD. Diagnosis and management of suspected cases of bioterrorism: A pediatric perspective. Pediatrics 2002;109:685-92.
Web sites providing information and guidelines on drugs related to pediatric disaster preparedness:
Positions and recommendations by the American Academy of Pediatrics
http://www.aap.org/terrorism/resources/federal_resources.html ![]() (last accessed 3/29/05)
(last accessed 3/29/05)
American College of Emergency Physicians
http://www.acep.org/1,2669,0.html ![]() (last accessed 3/29/05)
(last accessed 3/29/05)
Centers for Disease Control and Prevention
http://www.bt.cdc.gov/children/ ![]() (last accessed 6/16/05)
(last accessed 6/16/05)
FDA web site on drug preparedness and bioterrorism
http://www.fda.gov/Drugs/EmergencyPreparedness/BioterrorismandDrugPreparedness/default.htm ![]() (last accessed 3/29/05)
(last accessed 3/29/05)
Recommendations on flu pandemics by the Department of Health and Human Services
http://www.dhhs.gov/nvpo/pandemics/ ![]() (last accessed 3/29/05)
(last accessed 3/29/05)
Overview of FDA approved antiviral drugs for influenza treatment and prophylaxis
http://www.fda.gov/cder/drug/antivirals/influenza/default.htm ![]() (last accessed 3/29/05)
(last accessed 3/29/05)
CDC Information on national stockpile
http://www.bt.cdc.gov/stockpile/ ![]() (last accessed 6/16/05)
(last accessed 6/16/05)
“Mass casualty disaster plan checklist: A template for healthcare facilities” by the Association for Professional in Infection Control and Epidemiology
http://www.gnyha.org/eprc/general/templates/APIC_MassCasualtyChecklist.pdf ![]() (PDF) (last accessed 4/19/05)
(PDF) (last accessed 4/19/05)
Agency for Toxic Substances and Disease Registry (ATSDR): ”Medical management guidelines”
http://www.atsdr.cdc.gov/MHMI/mmg166.html#bookmark04 ![]() (last accessed 4/21/05)
(last accessed 4/21/05)
Center for Infectious Disease Research and Policy
Clinical pathway: Anthrax
http://www.cidrap.umn.edu/cidrap/files/17/anthrax-clinical-pathway.pdf ![]() (PDF) (last accessed 6/16/05)
(PDF) (last accessed 6/16/05)
Center for Infectious Disease Research and Policy
Clinical pathway: Botulism
http://www.cidrap.umn.edu/cidrap/files/19/botulism_clinical_pathway.pdf ![]() (PDF) (last accessed 6/16/05)
(PDF) (last accessed 6/16/05)
Center for Infectious Disease Research and Policy
Clinical pathway: Pneumonic Tularemia
http://www.cidrap.umn.edu/cidrap/files/28/tularemia-clin-path.pdf ![]() (PDF)(last accessed 6/16/05)
(PDF)(last accessed 6/16/05)
Center for Infectious Disease Research and Policy
Clinical pathway: Vesicular or pustular rash illness
http://www.cidrap.umn.edu/cidrap/files/18/smallpox_clinical_pathway.pdf ![]() (PDF) (last accessed 6/16/05)
(PDF) (last accessed 6/16/05)
Center for Infectious Disease Research and Policy
Clinical pathway: Viral hemorrhagic fever
http://www.cidrap.umn.edu/cidrap/files/25/vhf_clinical_pathway.pdf ![]() (PDF) (last accessed 6/16/05)
(PDF) (last accessed 6/16/05)
Center for Infectious Disease Research and Policy
Clinical pathway: Pneumonic Plague
http://www.cidrap.umn.edu/cidrap/files/22/plague_clinical_pathway.pdf ![]() (PDF) (last accessed 6/16/05)
(PDF) (last accessed 6/16/05)
Section 10. Psychosocial Needs of Children during Disasters
The Psychosocial Needs of Children during a Disaster
Draft for Public Comment
Purpose:
To properly care for children in hospitals it is necessary to consider both their physical and mental health needs and treating them in the context of the family unit. Children’s responses to disaster and hospitalization may share some aspects of adult responses, but are distinguished by the developmental contexts in which children of varying ages experience, mediate and communicate the impact of associated events and procedures. An unfamiliar environment such as a medical setting can be made to feel safer for pediatric visitors and patients by including familiar people, familiar things and routines. Hospitals need also note the cultural differences that may cause a group of children exposed to the same trauma to react differently and must ensure that mental health staff is sympathetic to each of these variances. Lastly, there are legal concerns regarding the treatment and release of children which each hospital should consider when creating the pediatric response portion of its disaster plan.
Section Contents:
- General Guidelines
- Development Specific Guidelines
- Infants
- Toddlers & Pre–School
- School Age
- Adolescents
- How Children Can React to a Disaster
- Age – specific reactions and signs of stress or illness
- Helpful Hints to Assist Children
- When to Consult a Mental Health Professional
- Legal Considerations
- Legal questions and issues that may arise during a disaster
- Cultural Differences about Death and Dying
- Obtaining Mental Health Services in the Community (LifeNet)
- Fact Sheet for Parents and Caregivers
- On-line Resources for Pediatric Psychosocial Issues
General Guidelines
- When describing the hospital experience to children of any age, it is important to be honest in your description and in answering any questions they may have. However, it is important not to give preconceived notions about what a child may feel. Caregivers should avoid the use of the words "pain" and "scary" in describing experiences the child may have since everyone feels pain and emotions differently.
- Since young children (preschool through school age) learn best by experience, provide as much information as you can to help the child learn about their upcoming experience. Describe what the child may smell, hear, touch, and feel using as many tangible items as possible, such as dolls and books.
- Children’s reactions and symptoms can be expressed through behavior, thoughts, emotions, and physical reactions. Children’s fears about their own safety can contribute to symptoms of anxiety and depression and may also lead to oppositional and aggressive behavior. This may be an attempt to reassert some sense of control and should be recognized as such.
- Don’t leave children unaccompanied in front of a television, for example with the news on, but allow them to talk about what is going on if they choose. Clarify misconceptions with simple, truthful explanations.
- Refrain from having conversations about the disaster in front of the children or within hearing distance. This can lead to misunderstandings and misconceptions.
- Gather unit staff and develop language for describing events of disaster. Ensure that all staff is educated accordingly and then communicate this information consistently to avoid adding to the children’s confusion.
- Opportunities for play are important for learning, expression of feelings, normalcy, escape and mastery. Age appropriate toys and diversionary activities are helpful to have on hand. This may include puzzles, books, simple art supplies and video and audiotapes. If possible allow children to interact in groups and monitor for misconceptions.
- Try not to separate from their primary caregivers for extended periods of time. Allow a parent/caregiver to accompany the child to procedures as much as possible. To encourage feelings of safety and familiarity try to limit the number of staff caregivers (i.e. assign same nurse to care).
- Parents will be most helpful when they are/feel informed- if they are upset from not knowing what is going on that tension is going to affect the child.
- Assess for any underlying mental health disorder that may require immediate psychiatric consultation such as trouble sleeping, lack of appetite and physical complaints with no medical basis.
- Gather information about varying cultural responses to trauma and death.
- Gather list of community resources (counseling services, etc) for distribution to parents/caregivers upon discharge.
- Identify staff within hospital who can assist with addressing the emotional and psychological issues i.e. social workers, psychologists, psychiatrists, chaplains, psychiatric nurses, etc and have an on-call list available for unit staff.
- Identify resources for staff support to cope with impact of seeing injured and/or dying children.
- Identify community resources that may be able to donate services, supplies, etc specifically for the children.
Development Specific Guidelines For Treating Children In The Hospital
Infants
- Try to let a parent/caregiver stay with the baby during medical procedures.
- Use familiar objects from home such as a stuffed animal, blanket, music box or toy to help comfort the baby before, during or after a procedure
Toddler and pre–school
- Try not to have conversations about your child's care in their presence unless you are including them in the conversation. Children overhear much more than adults think and without any explanation the information may seem terribly frightening.
- Let a parent/caregiver stay overnight with the child if possible. If appropriate, let other family members, including brothers and sisters, come and visit.
- Reassure child that the hospitalization is not a punishment. Try to avoid using good/bad labels particularly during a procedure. For example, instead of saying "See, you were so good, the doctor only had to do this once," you can say, "You did such a good job of sitting still, I know that was hard."
- Children learn best through play and “medical play” can be particularly useful. Allow them to handle some medical equipment such as a stethoscope, blood pressure cuff, etc. Allow them to practice the procedure on a doll.
- Allow child to make choices whenever possible but don't offer a choice when none exist. For example do not say, "Would you like to come into the treatment room now so the doctor can look at you?" It would better to say, "Do you want to bring your bear or blanket with you to the treatment room?"
School age
- School age children can be given more specific information about what is going to happen to them. Many medical terms can be confusing for children. For example, the term "I.V." could be confused with the word "ivy" or "dye" with "die." Give simple, specific explanations for procedures.
- This is a great age for medical play (communicating understanding, fears, etc. through play with medical equipment). Allow child the opportunity to reenact events through play with different kinds of toys or art materials. This is an important way for school age children to express their feelings and gain a sense of control over what is happening to them.
- Respect child's privacy and encourage others to do the same by knocking before entering the room and being sensitive to who is around when examinations are being conducted.
- Sometimes children at this age regress, or start up behaviors that they had grown out of (thumb sucking, bed wetting, etc.), when in a stressful situation like being in the hospital. Do not berate (come on, you’re a big girl now…) or punish for this behavior. Encourage child to express his feelings and discharge emotions through play.
Adolescents
- Try not to have conversations about teen’s care in his/her presence unless you are including him/her in the conversation. Adolescents can understand much more about their bodies and what is happening to them and may resent not being included in discussions about their condition or treatment.
- Do not assume that teens manage their emotions the same way as adults do. Give them opportunities to discuss what is happening with staff both with and without parent/caregiver being present so they can ask questions.
- Respect a teen’s privacy and encourage others to do the same by knocking before entering the room and being sensitive to who is around when examinations are being conducted.
How Children Can React To A Disaster
Children react differently to stressful events than adults. Their response can often be delayed and may be hard to detect. They may find it hard to talk about how they have been affected.
- Staff needs to be aware of changes in children’s behavior, like extra clinging or a change in appetite. Parents, teachers and other caring adults who know the child are in the best position to notice these changes.
- Don’t wait for them to come to you, ask questions like: Are they having trouble sleeping? Are they feeling less safe than before?
- Some children are more likely to have emotional reactions to the events:
- Children who witnessed the event firsthand or whose parent, relative of friend was killed or injured
- Children who are displaced from their home or schools
- Children who have a past history of emotional problems
- Children who have a past history of trauma, either as a victim or a witness to violence or abuse
- Children with an adult in their life who is having difficulty with their emotions, a witness to violence or victim of domestic violence
Emotional Responses also vary by development stages and may include the following:
Children aged 5 and younger may:
- Have fears of being separated from a parent
- Be unusually fearful, “fussy”, clingy, and have crying bouts
- Return to outgrown behavior, such as bed-wetting or baby talk
- Have nightmares or problems sleeping
- Have stomachaches, headaches or other physical complaints that do not have a medical base
- Startle easily
- Have a loss or increase in appetite
Children aged 6 to 11 may:
- Engage in repeated play that depicts the disturbing events over and over
- Have nightmares or problems sleeping
- Have unusual outbursts of anger
- Withdraw from friends and family
- Be fearful, anxious or preoccupied with safety and danger
- Return to behavior they have outgrown
- Express feelings of guilt
- Have frequent stomachaches, headaches or other physical complaints that do not have a medical base
- Have problems concentrating
- Experience persistent, disturbing feelings and memories when reminded of the event
Children aged 12 to 18 may:
- Have appetite changes
- Headaches, gastrointestinal problems
- Loss of interest in social activities
- Sadness or depression
- Feelings of inadequacy and helplessness
- Feelings of anger and aggression
- Isolation from others, less interests in friendships
- Repetitive behaviors such as hand–washing
Not all children exhibit all symptoms and their reactions may change over the first days or weeks following a crisis.
Helpful Hints To Assist Children During And After A Disaster
For children under age 5:
- Try to keep to normal routines and favorite rituals as much as possible
- Limit exposure to TV programs and adult conversations about the events
- Ask what makes them feel better
- Give plenty of hugs and physical reassurance
- Provide opportunities for them to be creative and find other ways to express themselves
For children older than age 5:
- Don’t be afraid to ask them directly what is on their mind and answer their questions honestly
- Talk to them about the news and any adult conversations they have heard
- Make sure they have opportunities to talk with peers if possible
- Set gentle but firm limits for acting out behavior
- Encourage verbal and play expression of thoughts and feelings
- Listen to child’s repeated retelling of the event
When To Consult A Mental Health Professional
Consultation with a mental health professional may be useful at any of these times. However, psychiatric consultation should be sought if any of the following is exhibited:
- Excessive fear of something terrible happening to their parents or loved ones
- Excessive and uncontrollable worry about things, such as unfamiliar people, places or activities
- Fear of not being able to escape if something goes wrong
- Suicidal thoughts or the desire to hurt others
- If the child has hallucinations
- Expressing feelings of being helpless, hopeless, and worthless
Legal Considerations
The following are legal questions and issues that may arise during a disaster. Having policies and procedures in place prior to an event should be considered.
- For unaccompanied children during a disaster, consent is not needed to treat for a life or limb-threatening situation. Is parental consent needed to treat a child victim with minor injuries? With psychological injuries?
- Is parental consent required to decontaminate an unaccompanied child? What if child is asymptomatic? What if child is refusing?
- What medical or social information can be released and to whom during a disaster?
- Check HIPAA rules and your legal counsel concerning the unidentified patient locator protocols, such as posting Polaroid photographs of unidentified children.
- Who can children be released to and if not the parent or caregiver, what permission or information is needed? What is your protocol for releasing children if no legal guardian or parent can be found or if no permission document is provided?
Cultural Differences About Death And Dying
Every culture has its own rituals and manner of mourning. Over time and through immigration and contact between different groups in the US, mourning patterns of ethnic groups have changed and continue to change all the time. Clinicians should be careful about definitions of “normality” in assessing families’ responses to death. Additionally, health care providers should remember not to assume people within any particular cultural group fit a pattern when mourning. Each family unit, as each individual, needs to be treated and assessed on an individual case–by–case basis.
- It is important for staff to appreciate an ethnic group’s particular attitudes about mourning and to find out from a family what its members believe about the nature of death, the rituals that should surround it, and the expectations of afterlife.
- Often a failure to carry out death rituals contributes to a family’s experience of unresolved loss.
- Helping family members deal with a loss often means showing respect for their particular cultural heritage and encouraging them actively to determine how they will commemorate the death of a loved relative.
- While it is generally better to encourage families toward openness about death, it is also crucial to respect their cultural values and timing for dealing with the emotional aftermath of a loss.
- Staff may inquire about:
- What are the prescribed rituals for handling dying, disposition of the body, rituals to commemorate the loss
- What are the group’s beliefs about what happens after death
- What do they believe about appropriate emotional expressions
- What are the gender rules for handling the death
- Staff should identify personnel in their setting who may be able to provide more details regarding specific cultural groups such as Pastoral Care, Social Work, or even particular staff members from various cultural groups.
Obtaining Mental Health Services In The Community
Every child experiences emotional difficulties from time to time, but at some point a child’s problems may warrant professional attention.
LifeNet
Counseling professionals provide free, confidential information and referral services, 24 hours a day. They have the latest information and where to go for help. Anyone can call. Help is available in several languages. They can also help find resources outside of NY State.
In English: 1-800-LIFENET (1-800-543-3638)
In Spanish: 1-877-AYUESE (1-877-298-3373)
In Chinese: ASIAN LIFENET (1-877-990-8585)
Contacting the child’s pediatrician for a referral to a mental health professional or clinic may also be helpful.
LifeNet Information may also be obtained at the NYC DOHMH web site:
http://www.nyc.gov/html/doh/html/cis/cis_lifenet.shtml ![]()
Fact Sheet After A Disaster: A Guide For Parents And Care–Givers From the National Institute of Mental Health
Natural disasters such as tornados, or man-made tragedies such as bombings, can leave children feeling frightened, confused, and insecure.
Whether a child has personally experienced trauma or has merely seen the event on television or heard it discussed by adults, it is important for parents, care-givers, and teachers to be informed and ready to help if reactions to stress begin to occur.
Children respond to trauma in many different ways. Some may have reactions very soon after the event; others may seem to be doing fine for weeks or months, then begin to show worrisome behavior. Knowing the signs that are common at different ages can help parents and teachers to recognize problems and respond appropriately.
Preschool Age
Children from one to five years in age find it particularly hard to adjust to change and loss. In addition, these youngsters have not yet developed their own coping skills, so they must depend on parents, family members, and teachers to help them through difficult times.
Very young children may regress to an earlier behavioral stage after a traumatic event. For example, preschoolers may resume thumb sucking or bedwetting or may become afraid of strangers, animals, darkness, or "monsters." They may cling to a parent or teacher or become very attached to a place where they feel safe.
Changes in eating and sleeping habits are common, as are unexplainable aches and pains. Other symptoms to watch for are disobedience, hyperactivity, speech difficulties, and aggressive or withdrawn behavior. Preschoolers may tell exaggerated stories about the traumatic event or may speak of it over and over.
Early Childhood
Children aged five to eleven may have some of the same reactions as younger boys and girls. In addition, they may withdraw from play groups and friends, compete more for the attention of parents, fear going to school, allow school performance to drop, become aggressive, or find it hard to concentrate. These children may also return to "more childish" behaviors; for example, they may ask to be fed or dressed. Do boys and girls act differently?
Adolescence
Children twelve to fourteen are likely to have vague physical complaints when under stress and may abandon chores, school work, and other responsibilities they previously handled. While on the one hand they may compete vigorously for attention from parents and teachers, they may also withdraw, resist authority, become disruptive at home or in the classroom, or even begin to experiment with high-risk behaviors such as drinking or drug abuse. These young people are at a developmental stage in which the opinions of others are very important. They need to be thought of as "normal" by their friends and are less concerned about relating well with adults or participating in recreation or family activities they once enjoyed.
In later adolescence, teens may experience feelings of helplessness and guilt because they are unable to assume full adult responsibilities as the community responds to the disaster. Older teens may also deny the extent of their emotional reactions to the traumatic event.
How to Help
Reassurance is the key to helping children through a traumatic time. Very young children need a lot of cuddling, as well as verbal support. Answer questions about the disaster honestly, but don’t dwell on frightening details or allow the subject to dominate family or classroom time indefinitely. Encourage children of all ages to express emotions through conversation, drawing, or playing and to find a way to help others who were affected by the disaster.
Try to maintain normal routines and encourage children to participate in enjoyable activities. Reduce expectations temporarily about performance in school or at home, perhaps by substituting less demanding responsibilities for normal chores.
Finally, acknowledge that you, too, may have reactions associated with the traumatic event, and take steps to promote your own physical and emotional healing.
When to Seek More Help
Consultation with a mental health professional may be useful at any of these times. However, psychiatric consultation should be sought if any of the following is exhibited:
- Excessive fear of something terrible happening to their parents or loved ones
- Excessive and uncontrollable worry about things, such as unfamiliar people, places or activities
- Fear of not being able to escape if something goes wrong
- Suicidal thoughts or the desire to hurt others
- If the child has hallucinations
- Expressing feelings of being helpless, hopeless, and worthless
On–Line Resources For Pediatric Psychosocial Issues
American Academy of Pediatrics
AAP Children, Terrorism and Disaster. Web site created by AAP. Useful with multiple documents related to children’s needs during disasters.
http://www.aap.org/terrorism/index.html ![]()
Child Deaths Hit Communities Hard: Disasters Demand Psychological Triage
AAP News Article
http://aapnews.aappublications.org/content/vol14/issue5/ ![]()
The Child’s Loss: Death, Grief and Mourning: How Caregivers Can Help Children Exposed to Traumatic Death. From the Child Trauma Academy
http://www.childtrauma.org/ctamaterials/loss care f1 02.pdf ![]()
Clinical Work with Culturally Diverse Dying Patients
http://www.angelfire.com/on/NYCLTCethicsnetwork/econgress.html ![]()
Family Readiness Kit-Preparing to Handle Disaster
The American Academy of Child and Adolescent Psychiatry has suggestions for “Helping Children after a Disaster.”
http://www.aacap.org/publications/factsfam/disaster.htm ![]()
Federal Emergency Management Agency (FEMA) for Kids
Site with multiple games, coloring books, and materials aimed at younger, computer savvy children.
www.fema.gov/kids ![]()
How Pediatricians Can Respond to the Psychosocial Implications of Disasters
AAP Policy statement
http://aappolicy.aappublications.org/ ![]()
National Advisory Committee on Children and Terrorism
http://www.bt.cdc.gov/children/ ![]()
National Institute of Cancer – Loss, Grief and Bereavement
http://www.cancer.gov/cancertopics/pdq/supportivecare/bereavement/healthprofessional ![]()
National Child Traumatic Stress Network
http://www.nctsnet.org/nccts/nav.do?pid=hom_main ![]()
National Mental Health Information Center
Publications on Disaster and Trauma
http://mentalhealth.samhsa.gov/publications/Publications_browse.asp?ID=181&Topic=Disaster%2FTrauma ![]()
New York State Office of Mental Health
www.omh.state.ny
New York University Child Study Center
www.aboutourkids.org ![]()
Pediatrician’s Role in Disaster Preparedness (AAP policy statement)
http://aappolicy.aappublications.org/ ![]()
Perry. BD. Helping Traumatized Children: A Brief Overview for Caregivers. Child Trauma Academy
http://www.childtrauma.org/index.php/articles/articles-for-caregivers ![]()
Psychosocial Issues for Children and Families in Disasters: A Guide for the Primary Care Physician
Joint publication between AAP and US Center for Mental Health Services
http://mentalhealth.samhsa.gov/publications/allpubs/SMA95-3022/default.asp ![]()
Terrorist Attacks and Children
Article found at the National Center for Post Traumatic Stress Disorder
http://www.ptsd.va.gov/professional/pages/terrorist_attacks_and_children.asp ![]()
Tips for Talking About Disasters
National Mental Health Information Center
http://www.mentalhealth.samhsa.gov/cmhs/EmergencyServices/after.asp#children ![]()
Section 11. Pediatric Infection Control Considerations
Pediatric Infection Control Considerations
Draft for Public Comment
Purpose:
The following recommendations are based on limited published materials concerning infection control information that is specifically applicable to hospital management of a large influx of children (and accompanying adults) affected by a biological disaster. The very basic infection control guidance that follows is structured to address the infection control needs of two populations of concern in a pediatric emergency:
- Exposed/symptomatic children
- Exposed/asymptomatic children
Section Contents:
- General Guidelines
- Recommendations for use of authoritative guidance documents for infection control measures for the pediatric population
- Infection Control Measures for Exposed/Asymptomatic Children
- Infection Control Measures for Exposed/Symptomatic Children
- Co-horting Children in a Hospital Setting
- Environmental Measures for Pediatric Units
- Staff Child Ratio and Group Size Indicator
General Guidelines:
For all children who are symptomatic owing to a biological event, use applicable HICPAC Guidelines (currently:1996 Guidelines for Isolation Precautions in Hospitals); @ http://www.cdc.gov/hicpac/2007IP/2007isolationPrecautions.html ![]() )
)
- For asymptomatic infants, toddlers, and other children requiring diapering, feeding, toileting, and assistance with hand hygiene: use guidelines that are applicable to day care settings (see: US Department of Health and Human Services web site: “13 Indicators of Quality Child Care Research Update 2002” @ http://aspe.hhs.gov/hsp/ccquality-ind02/
 ).
).
Infection Control Measures for Exposed/Symptomatic children:
- HICPAC Isolation guidelines apply: appropriate to the nature of the illness/exposure;
- Cohort as necessary (same exposure/same symptoms);
- It is not practical to place masks on infants or young children to contain respiratory droplets/droplet nuclei: substitute hand hygiene/face washing/nose wiping;
- It is not practical to place infants or young children in portable isolation units alone to contain respiratory droplets/droplet nuclei;
- Young children and infants should not be left alone. Adult care givers of children placed in isolation should be instructed in appropriate infection control measures such as doffing and donning of gowns, gloves, and masks, hand hygiene and cough etiquette. Staff should insure that adult care givers are following appropriate infection control measures.
Infection Control Measures for Exposed/Asymptomatic Children:
- Promptly evaluate and separate as soon as possible from symptomatic children and symptomatic adults;
- Similarly exposed/asymptomatic children may be co-horted.
- Day Care approaches (see the DHHS document) apply;
- Hand Hygiene is paramount;
- As a priority: educate emergency care givers about sanitary considerations.
Cohorting of Children in a Hospital Setting:
- Ideally cohort according to age group to accommodate sanitary needs of infants and young children (diapering, toileting, hand hygiene, feeding; cleaning);
- Traumatized children may regress under duress and may require additional help with sanitary needs;
- Smaller group size is associated with a lower risk of infection in child care settings (DHHS document p. 16);
- Support infection control by aiming for recommended age appropriate staff: child ratios. (see DHHS p. 15: “Staff Child Ratio and Group Size Indicator)
Environmental Measures for Pediatric Units:
- Establish hand hygiene procedures and ensure adequate supplies of soap, sinks, paper towels;
- For infants/young children: establish diapering protocols;
- For infants/young children: use the HHS document (or similar) for guidance re: setting up sanitary changing stations;
- For young children: toys should be easy to clean (hard plastic not fuzzy);
- For young children: assign individual sleeping mats (if used);
- For infants/young children: adequate clean linens, disposable diapers, changes of clothing;
- Waste/soiled linen collection units should be child safe, adequate in number, constructed to permit hands free use;
- Have adequate supplies of cleaning/disinfecting materials stored in a child safe manner;
- Have cleaning/disinfection procedures and schedules in place for toilets, bathrooms, changing stations, sleeping mats, toys, etc. Any restrictions on disinfectant used?
- Any reusable equipment or toys should be appropriately cleaned following hospitals Infection Control procedures, or as recommended for the agent of concern.
Staff Child Ratio And Group Size Indicator
From US Department of Health and Human Services web site: “13 Indicators of Quality Child Care Research Update 2002” http://aspe.hhs.gov/hsp/ccquality-ind02/#Staff1 ![]() accessed June 15, 2005.
accessed June 15, 2005.
These indicators only have one standard represented because in the national data base a specific state regulation that deals with staff child ratio and group size exists. Even so, the variation of these regulations among the states is great. While some states meet or almost meet these standards for staff child ratio and group size, many states do not. Of all the indicators, the greatest variation occurs in how state regulations match up with the national standard for staff child ratio and group size.
CFOC Standard (1992):
ST 002–Child: staff ratios for centers and large family child care homes shall be maintained as follows during all hours of operation:
| Age | Child–staff ratio | Maximum group size |
|---|---|---|
| Birth–12 months | 3:1 | 6 |
| 13–24 months | 3:1 | 6 |
| 25–30 months | 4:1 | 8 |
| 31–35 months | 5:1 | 10 |
| 3 year olds | 7:1 | 14 |
| 4 year olds | 8:1 | 16 |
| 5 year olds | 8:1 | 16 |
| 6–8 year olds | 10:1 | 20 |
| 9–12 year olds | 12:1 | 24 |
When there are mixed age groups in the same room, the child:staff ratio and group size shall be consistent with the age of the majority of the children when no infants or toddlers are in the mixed age group. When infants or toddlers are in the mixed age group, the child:staff ratio and group size for infants and toddlers shall be maintained.
Research Review/Gap Analysis:
Review of all the major research in child care clearly demonstrates the importance of maintaining appropriate child:staff ratios and group sizes. Child:staff ratios and group sizes are two of the best indicators for determining the quality of a child care program and they significantly affect many other health and safety issues. Smaller group size is associated with a lower risk of infection in child care. The risk of illness in children between the ages of one and three years of age increases as the group size increases to four or more, whereas children in groups of three or fewer have no more risk of illness than children cared for at home (Bartlett, Orton, & Turner, 1986; Bell, Gleiber, Mercer, Hifer, Guinter, Cohen, Epstein, & Narayanan, 1989). The risk of repeated ear infections increases in one- to six-year-old children who attend child care in groups of more than six children (Hardy & Fowler, 1993).
The risk of Haemophilus influenza infections increases for children one year of age or older in a child care setting with four or more children, and the risk of infection peaks in settings with 21 or more children. Research indicates that group size should be limited to twice the maximum number of children allowed per adult. Smaller child care centers, not just those with smaller class sizes, have lower rates of disease. Outbreaks of Hepatitis A occur at the rate of 3% in centers that enroll less than 20 children but 53% in those that enroll 51 or more children (Hadler, Erben, Francis, Webster & Maynard, 1982). Children in small child care centers in France had two to three times the risk of repeated infections (e.g., upper respiratory tract infections, otitis media, conjunctivitis) than children in family child care settings with no more than three children (Collet, Burtin, Kramer, Bossard & Ducruet, 1994).
Lower child: staff ratios reduce the transmission of disease. Although there is little research available that examines the relationship between particular child:staff ratios and children’s health (a major gap that needs to be addressed), the research that is available suggests that fewer children per adult reduces the transmission of disease because caregivers are better able to monitor and promote healthy practices and behaviors (Bredekamp, 1990; Hayes, Palmer, & Zaslow, 1990).
Appendix A: New York City Specific Resources
Table A-1 New York City Hospital Pediatric Intensive Care Unit Bed Capacity, August 2004 Critical Asset August 2004 Critical Asset HERDS Survey
| County | Hospital | Pediatric ICU Beds Certified | Pediatric ICU Beds Staffed | Pediatric ICU Bed Surge |
|---|---|---|---|---|
| Bronx | Jacobi Medical Center | 6 | 4 | 4 |
| Bronx | Lincoln Medical & Mental Health Center | 8 | 8 | 0 |
| Bronx | Montefiore Medical Center Henry & Lucy Moses Div | 14 | 0 | |
| Kings | Brookdale Hospital Medical Center | 5 | 5 | 0 |
| Kings | Kings County Hospital Center * | 87 | 87 | 0 |
| Kings | Long Island College Hospital | 5 | 5 | 5 |
| Kings | Maimonides Medical Center | 11 | 11 | 0 |
| Kings | New York Methodist | 5 | 5 | 10 |
| Kings | University Hospital Of Brooklyn | 5 | 5 | 0 |
| New York | Bellevue Hospital Center | 5 | 4 | 1 |
| New York | Beth Israel Medical Center – Petrie Campus | 5 | 2 | 0 |
| New York | Harlem Hospital Center | 6 | 6 | 2 |
| New York | Metropolitan Hospital Center | 4 | 4 | 0 |
| New York | Mount Sinai Hospital | 16 | 16 | 3 |
| New York | New York Presbyterian Hospital Columbia Presbyterian Center** | 28 | 28 | 5 |
| New York | New York Presbyterian Hospital New York Weill Cornell Center | 20 | 20 | 5 |
| New York | NYU Hospitals Center | 9 | 9 | |
| New York | SVCMC–St Vincent's Manhattan | 4 | 4 | 0 |
| Queens | Jamaica Hospital Medical Center | 3 | 3 | 1 |
| Queens | Long Island Jewish Medical Center** | 12 | 12 | 8 |
| Queens | New York Hospital Medical Center Of Queens | 4 | 4 | 1 |
| Richmond | SVCMC–St Vincent's Staten Island | 2 | 2 | 0 |
| Richmond | Staten Island University Hospital–North | 4 | 4 | 2 |
| Total | Hospitals with PICU 23 | 268 | 248 | 47 |
* KCHC included NICU in this total
** NYS Designated Pediatric Trauma Centers
Appendix A-2 Map of New York City Resources